Supplement-Drug Interaction Checker
Check for potential interactions between your medications and supplements. This tool uses clinical-grade interaction data to help you avoid dangerous combinations. Note: This is not a substitute for professional medical advice.
Interaction Results
Every year, millions of people take prescription drugs along with dietary supplements-vitamins, herbs, minerals, and more. But here’s the problem: supplement drug interactions are rarely discussed during doctor visits. Patients don’t mention them. Doctors don’t always ask. And when interactions happen, they can be serious-sometimes deadly.
A 2015 study in JAMA Internal Medicine found that supplement-drug interactions send about 23,000 people to the emergency room every year in the U.S. alone. That’s not a small number. It’s not rare. And it’s preventable-if you know how to check.
This isn’t about guessing. It’s not about trusting a label or assuming something is "natural" so it’s safe. It’s about using the right tools, the right way. If you’re a patient, caregiver, or healthcare provider, learning how to check supplements in drug interaction databases can save lives.
Why Most People Get This Wrong
Many assume that because supplements are sold over the counter, they’re harmless. That’s dangerous thinking. Ginkgo biloba, for example, is a popular herbal supplement. But if you’re taking warfarin or apixaban, it can increase your risk of bleeding. Milk thistle might help your liver, but it can interfere with how your body processes certain antidepressants or chemotherapy drugs.
Here’s the real issue: patients don’t tell their doctors. A 2022 study in JAMA Network Open found that only 37% of patients disclose supplement use during medical visits. Why? They don’t think it’s important. They think their doctor doesn’t care. Or they just forget.
Doctors, on the other hand, often don’t have the right tools. Many use general drug interaction checkers designed for prescription medications-not supplements. These tools miss up to 80% of supplement-related risks because they don’t break down ingredients. They see "milk thistle" and stop there. But what if the bottle also contains black pepper extract to boost absorption? That’s piperine-and piperine can slow down how fast your body clears drugs like statins or blood pressure meds.
That’s why you need a database built for supplements-not just drugs.
What Makes a Good Supplement Interaction Database
Not all databases are created equal. Some track thousands of drug-drug interactions but barely mention supplements. Others are outdated. The best ones have three things:
- Ingredient-level detail: They don’t just list "coenzyme Q10." They list every form, dosage, and brand-specific blend.
- Clear severity ratings: Not all interactions are equal. Some are minor. Some can kill you.
- Management advice: It’s not enough to say "avoid." You need to know what to do instead.
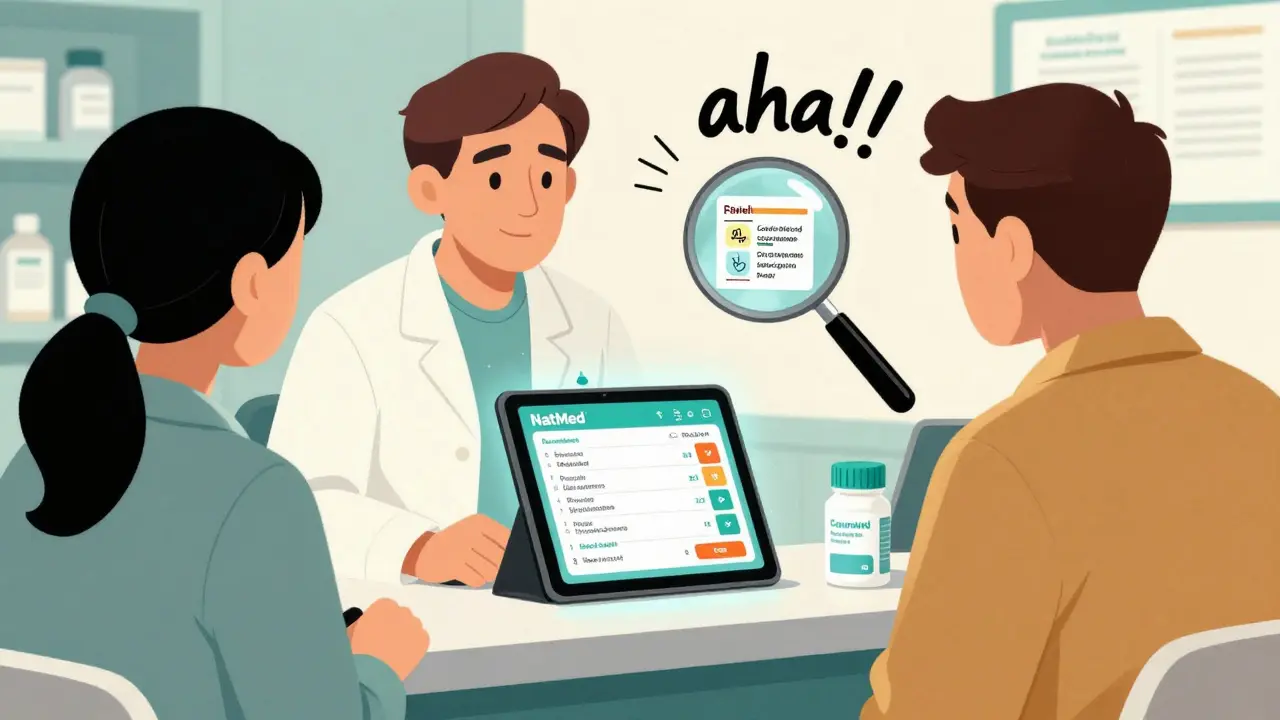
The gold standard is NatMed (a clinical decision support system developed by Natural Medicines, with over 1,900 supplement monographs and 51,000+ commercial product formulations mapped to active ingredients). It’s used in 78% of U.S. hospitals and trusted by oncology teams because of its 94.3% inter-rater reliability among pharmacists.
Other tools like DrugBank and FDB’s MedKnowledge are strong for drug-drug interactions but fall short on supplements. DrugBank has over 14,000 nutrient-drug pairs, but only 42% explain the mechanism. FDB covers 2,400 supplements-good, but NatMed covers nearly 2,000 unique supplements with full ingredient breakdowns.
And then there’s PHYDGI, which focuses only on herbal interactions and rates them on a 0-10 scale for strength. Useful for specialists, but not for general use.
Bottom line: If you’re checking supplements, use NatMed. If you can’t access it, ask your pharmacist. They likely have a subscription.
Step-by-Step: How to Check Supplement Interactions
Here’s exactly how to do it-whether you’re a patient or a provider.
- Collect every supplement you’re taking. Don’t guess. Look at the bottles. Write down the full name, dosage, and how often you take it. Include vitamins, herbal teas, protein powders, fish oil, melatonin, and even probiotics. Some people forget these are supplements too.
- Check the ingredient list. Many supplements contain proprietary blends. That means the label says "energy blend: 500 mg"-but doesn’t say what’s in it. If you can’t find the exact ingredients, call the manufacturer or search the product online. The FDA found that 68% of supplement products contain unlisted ingredients. Don’t trust the label.
- Write down all your prescription and over-the-counter drugs. Include antibiotics, painkillers, blood pressure meds, antidepressants, and even antacids. Even a single pill can interact.
- Go to a reliable database. Open NatMed (if you have access). If not, ask your pharmacist to run the check. Type in each supplement by its active ingredient-not the brand name. For example, type "ginkgo biloba," not "GinkgoMax 120 mg." Then add each drug you take.
- Look at the severity rating. NatMed uses four levels: Contraindicated (don’t combine), Major (high risk), Moderate (monitor), and Minor (low risk). If you see "Contraindicated" with warfarin and ginkgo, stop taking ginkgo immediately and call your doctor.
- Read the management advice. Good databases don’t just warn you-they tell you what to do. For example: "Switch to vitamin K2 instead of vitamin K3 if on anticoagulants," or "Take St. John’s wort 4 hours apart from your antidepressant." Follow that advice.
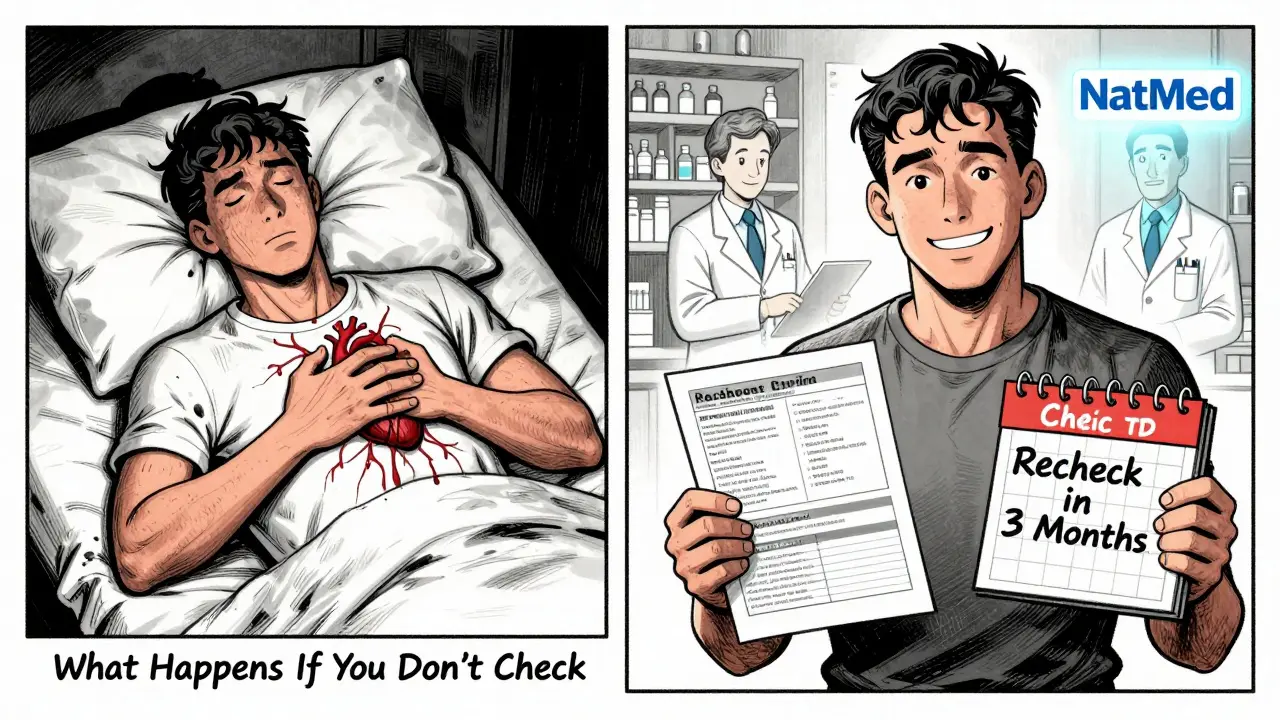
- Recheck every 3 months. Supplements change. Brands reformulate. New studies come out. A supplement that was safe last year might not be now.
Real Cases Where This Saved Lives
In 2023, a 78-year-old man at Johns Hopkins Hospital was on apixaban for atrial fibrillation. He started taking ginkgo biloba for memory. His pharmacist ran a check in NatMed and found a Major interaction: increased bleeding risk. The patient didn’t know ginkgo could thin his blood. They stopped it. No bleed. No hospitalization.
Another case: a woman on chemotherapy for breast cancer was taking turmeric capsules for inflammation. Her oncology nurse used NatMed and found that curcumin can interfere with taxanes-drugs she was receiving. The supplement was replaced with a safe anti-inflammatory. Her treatment stayed on track.
These aren’t outliers. They’re routine now in hospitals that use proper databases.
What to Do If You Can’t Access NatMed
You don’t need a hospital account to get help. Here’s what you can do:
- Ask your pharmacist. Most community pharmacies have access to NatMed or similar tools. They can run the check for free.
- Use DrugBank’s public version. It’s not as deep on supplements, but it’s better than nothing. Search by ingredient name.
- Call the National Institutes of Health’s Office of Dietary Supplements. They offer free fact sheets on common supplement-drug interactions.
- Use the LiverTox database from NIH if you’re taking supplements and have liver concerns. It now includes supplement-induced liver injury data as of 2024.
Don’t rely on Google. Don’t trust Reddit. Don’t assume your friend’s experience applies to you. Use evidence-based tools.
Common Mistakes and How to Avoid Them
Here are the top 5 errors people make:
- Using brand names instead of ingredients. "I take Nature Made Omega-3." The database needs "omega-3 fatty acids" or "EPA/DHA." Always use the active compound.
- Ignoring proprietary blends. If the label says "proprietary blend," you’re flying blind. Look up the brand online. Find the full ingredient list.
- Thinking "natural" means safe. Foxglove is natural. It’s also digitalis-a potent heart drug. Many herbal supplements contain plant compounds that act like pharmaceuticals.
- Not checking regularly. Your meds change. Your supplements change. Recheck every time you get a new prescription or start a new supplement.
- Assuming your doctor knows. Even if you told them, they might not have the right tool. Be your own advocate. Bring the list. Ask: "Can we check this for interactions?"
What’s Changing in 2026
The field is moving fast. In 2024, NatMed rolled out AI-powered name recognition that cuts false negatives by 37%. That means if you type "ginkgo leaf extract," it now finds "ginkgo biloba" even if you’re not exact.
FDB is integrating with Epic EHR systems so alerts pop up automatically when a doctor prescribes a drug that clashes with a supplement you’ve logged. That’s coming to major hospitals by late 2024.
The FDA is piloting blockchain verification for supplement ingredients. Imagine scanning a QR code on your bottle and seeing exactly what’s inside-verified by the manufacturer. That’s real, and it’s rolling out in 2025.
But here’s the bottom line: none of this matters if you don’t check. The technology is there. The data is there. The warnings are there. You just need to use them.
Final Advice: Don’t Wait for a Crisis
If you’re on more than one prescription and take any supplement-vitamins, herbs, fish oil, melatonin, ashwagandha, CBD-you need to run this check. Now. Not tomorrow. Not next month.
Supplement-drug interactions don’t always cause immediate symptoms. Sometimes, they build up. A slow rise in blood pressure. A drop in kidney function. A sudden bleed. By the time you feel it, it’s too late.
Use the tools. Ask the pharmacist. Write down what you take. Recheck every three months. Your life might depend on it.