Starting a new medication can feel overwhelming. You’ve got a prescription in hand, maybe a handful of pills in a plastic bottle, and a doctor’s voice echoing in your head: "Take this once a day." But what does that really mean? When? With food? What if you miss one? What happens if you accidentally grab the wrong bottle? These aren’t just questions-they’re safety concerns that affect millions of first-time patients every year.
Medication errors are more common than most people realize. In the U.S. alone, over 1.3 million emergency room visits each year are caused by bad reactions to medicines. About 350,000 of those lead to hospital stays. And here’s the scary part: up to half of these errors are preventable. That means if you know what to look for, you can protect yourself-and even save your life.
Know the Six Rights of Medication Safety
Healthcare professionals use a simple checklist called the Six Rights to avoid mistakes. As a patient, you should use it too. It’s not complicated, but it’s powerful.
- Right patient: Make sure the name on the bottle matches yours. Hospitals and pharmacies use two identifiers-your full name and date of birth-to confirm this. At home, double-check the label before you take anything.
- Right medication: Does the pill look the same as last time? Generic versions often change color or shape, even if they work the same. If something looks off, ask your pharmacist.
- Right indication: Why are you taking this? Don’t assume. If your doctor says it’s for high blood pressure, but the bottle says "for pain," ask. Misunderstanding the purpose is a leading cause of misuse.
- Right dose: Never guess. A teaspoon is not a measuring spoon. Use the dosing cup, syringe, or dropper that came with the medicine. Household spoons vary by 25-50%, and that difference can be dangerous.
- Right route: Is it meant to be swallowed, placed under the tongue, applied to the skin, or injected? Taking a cream orally or a pill as a suppository can cause serious harm.
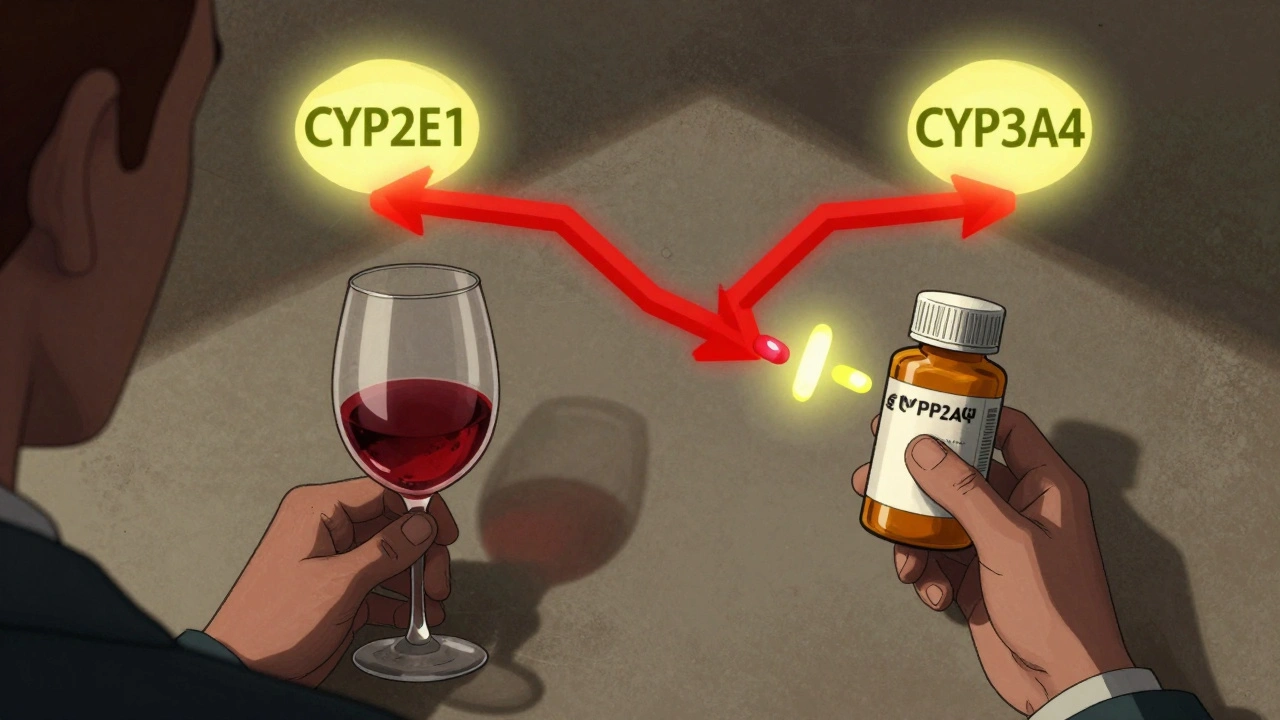
- Right time: Some meds need to be taken with food to avoid stomach upset. Others must be taken on an empty stomach. Some work best in the morning; others at night. Ask your pharmacist about timing and food interactions.
Keep a Complete Medication List
Most people don’t realize they’re taking more than they think. It’s not just prescriptions. It’s the ibuprofen you take for headaches, the melatonin for sleep, the fish oil, the vitamin D, even the herbal teas. All of them can interact.
Doctors and pharmacists need to see your full list-not just the big ones. A 2022 study found that patients who kept a complete, up-to-date list had 27% fewer medication errors. That’s huge.
Here’s what to include:
- Brand and generic names
- Dose (e.g., 10 mg, 5 mL)
- How often (once daily, twice a week, etc.)
- Why you’re taking it
- When you started
- Pharmacy name and phone number
Keep this list in your wallet, on your phone, and printed out. Bring it to every appointment-even if you think nothing changed. A simple 5-minute review can catch a dangerous interaction before it happens.
Never Take Someone Else’s Medicine
"My friend takes this for anxiety and it helped her-maybe it’ll help me too." This is a dangerous myth.
The FDA says sharing medications causes about 8% of emergency visits for drug reactions. Why? Because what works for one person can harm another. A pill that lowers blood pressure for someone with hypertension could crash your heart rate if you don’t have high blood pressure. Antibiotics prescribed for a sinus infection won’t treat your ear infection-and might make future infections harder to treat.
Even if the pill looks identical, the dosage, filler ingredients, or release mechanism may be different. Never take anything not prescribed to you.
Store Medications Correctly
Not all pills belong in the bathroom cabinet. Heat, moisture, and light can break down medicine before its expiration date.
- Insulin: Must be refrigerated (36-46°F / 2-8°C) until opened. After opening, it can stay at room temperature for up to 28 days.
- Most oral pills: Keep below 86°F (30°C), away from humidity. The bathroom is a bad choice. A bedroom drawer or kitchen cabinet away from the stove is better.
- Liquid antibiotics: Often need refrigeration. Check the label. If you leave them out too long, they lose strength-and you risk treating an infection poorly.
- Controlled substances (like opioids or ADHD meds): Lock them up. These are targeted by thieves and can be dangerous if found by children or teens.
Check expiration dates. A 2023 Merck report found that 18% of medication errors came from using expired drugs-especially liquid forms and antibiotics. If it’s past the date, don’t risk it. Return it to your pharmacy for safe disposal.
Read the Label-In Good Light
Over 15% of medication errors happen because someone misread the label. It’s dark. You’re tired. The print is small. You grab the bottle and take a pill without reading.
Always turn on the light. Use reading glasses if you need them. Don’t rush. Look for:
- Drug name (brand and generic)
- Strength
- Directions (how much, how often)
- Warnings ("Do not drink alcohol," "May cause drowsiness")
- Expiration date
If you can’t read it, call your pharmacy. They’ll send you a larger print version or explain it over the phone.
Ask Questions-Even If You Feel Awkward
Most patients don’t ask enough questions. A 2022 study showed that patients who asked three or more questions about a new medication had 34% fewer side effects in the first month.
Here are the questions you should always ask:
- "What should I do if I miss a dose?" (Only 22% of patients ask this, but it’s critical.)
- "How should I store this?" (40% of medications have specific storage needs.)
- "What side effects should I watch for?" (Only 65% of pharmacy consultations cover this.)
- "Can this interact with anything else I take?"
- "Is there a cheaper or generic version?"
- "What happens if I stop taking it?"
Pharmacists are trained to help you understand your meds. They’re not busy people who just hand out pills-they’re your medication safety partners.
Use Tools to Stay on Track
Forgetting a dose is one of the most common mistakes. A 2022 study found that first-time users who used a medication reminder app improved their adherence by 28%.
Apps like Medisafe and MyMeds let you:
- Scan the barcode on your pill bottle to auto-fill details
- Set alarms for each dose
- Get alerts if you’re due for a refill
- Share your schedule with a family member
These apps are especially helpful if you take five or more medications. They reduce the mental load so you don’t have to remember everything.

Watch for Changes-And Speak Up
Your body reacts differently to new drugs. Some side effects are normal. Others are warning signs.
Call your doctor immediately if you notice:
- Severe rash, swelling, or trouble breathing
- Unusual bleeding or bruising
- Extreme dizziness or confusion
- Signs of an allergic reaction (hives, tight throat, swelling of face or tongue)
- Any new symptom that feels "not right"
Don’t wait to see if it goes away. Early action can prevent hospitalization.
What Happens When You Leave the Hospital?
One of the riskiest moments for medication errors is right after you leave the hospital. A 2023 report found that 22% of errors happen during discharge.
Why? You’re overwhelmed. You get a stack of papers. You’re told to start three new drugs and stop two others. No one explains how.
Before you leave, ask:
- "Can you walk me through every change to my meds?"
- "Can I get a printed list of what I’m taking now?"
- "Who should I call if I have questions after I get home?"
Don’t leave without this information. It’s your right.
It Takes Time-Be Patient With Yourself
Building a safe medication routine doesn’t happen overnight. A 2023 University of Michigan study found it takes most people 2-3 weeks to feel confident. That’s normal.
Use the tools. Ask questions. Write things down. Keep your list updated. Don’t be embarrassed to say, "I don’t understand."
Medication safety isn’t about being perfect. It’s about being aware. It’s about asking for help when you need it. And it’s about knowing that you have the power to protect yourself.