When it comes to prescribing medications, especially generics, the old model-where a doctor makes the decision alone-isn’t cutting it anymore. Too many patients are stuck with confusing pill schedules, avoidable side effects, or sky-high drug bills. But there’s a better way: team-based care. It’s not just a buzzword. It’s a system where doctors, pharmacists, nurses, and care coordinators work together to make sure patients get the right meds at the right price. And when it comes to generic prescribing, this approach saves money, reduces errors, and actually improves health outcomes.
Why Generic Prescribing Needs a Team
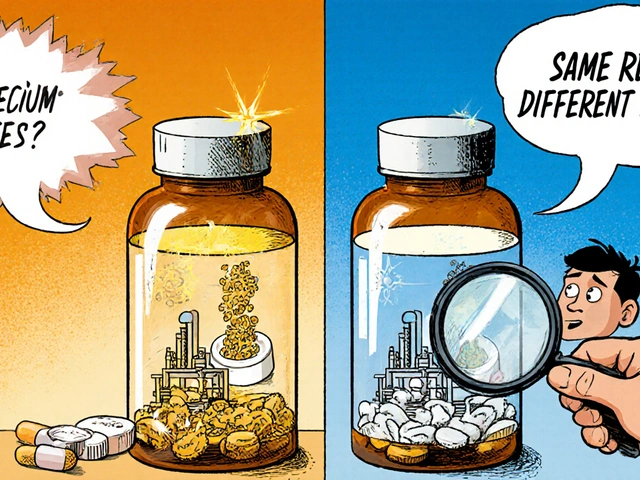
Generic drugs work just like brand-name versions. They have the same active ingredients, same dosages, same safety profiles. Yet, many patients never get offered them. Why? Because prescribing isn’t just about medical knowledge-it’s about time, communication, and cost awareness. A doctor might see 30 patients a day. They’re juggling diagnoses, lab results, and insurance forms. They don’t have time to check every drug’s generic alternative, compare prices, or explain why switching makes sense. Enter the pharmacist. Trained specifically in medication use, pharmacists spot opportunities for generic substitution that a busy physician might miss. In one study, pharmacists integrated into care teams increased appropriate generic use by 28%. That’s not just saving patients money-it’s improving adherence. When a patient sees their monthly insulin bill drop from $450 to $120, they’re far more likely to take it regularly.Who’s on the Team and What Do They Do?
Team-based care isn’t random. It’s structured. Each member has a clear role:- Physicians handle complex diagnoses, adjust treatment plans for multiple conditions, and approve final medication changes.
- Pharmacists conduct full medication reviews, identify drug interactions, suggest cost-effective generics, and counsel patients on proper use.
- Nurses and Medical Assistants monitor chronic conditions like diabetes or hypertension, track adherence, and flag issues before they become emergencies.
- Care Coordinators make sure everyone’s on the same page-linking primary care with specialists, managing referrals, and updating electronic records.
How It Works in Practice
Imagine a 68-year-old with hypertension, type 2 diabetes, and high cholesterol. They’re on seven medications. One’s a brand-name statin costing $300/month. Another is a brand-name antihypertensive. Their out-of-pocket costs are eating into their Social Security check. In a traditional model, the doctor might stick with what’s familiar-or what’s easiest to prescribe. But in a team-based setting:- The pharmacist runs a comprehensive medication review and finds three generics that are clinically equivalent.
- The nurse checks blood pressure logs and notices the patient hasn’t filled their last script in six weeks.
- The care coordinator pulls up their insurance formulary and confirms the generics are covered at Tier 1.
- The doctor approves the switch during a brief follow-up.

Proof It Works
The numbers don’t lie. According to data from the National Center for Biotechnology Information, team-based medication management reduces hospital readmissions by 17.3% and cuts duplicative testing by 22.8%. PureView Health Center found that per-patient annual savings from optimized generic prescribing and avoided complications range from $1,200 to $1,800. One patient review on Healthgrades said: “The pharmacist caught three medication interactions my doctor missed and switched me to generics that saved me $200 monthly.” That’s not luck. That’s system design. Medicare Part D’s Medication Therapy Management (MTM) program-launched in 2003-is now serving over 12 million beneficiaries. And since 2023, eligibility expanded to include patients on just four or more medications, not five. That means millions more will get this level of scrutiny.Challenges? Yes. But They’re Solvable
It’s not perfect. Some doctors resist giving up control. One physician on Doximity admitted that setting up team-based care initially added 2.5 hours to their week. That’s because workflows aren’t built overnight. There’s also tech friction. If the EHR doesn’t connect the pharmacist’s notes to the doctor’s chart, recommendations get lost. And in smaller practices, documentation gaps increase liability risk by nearly 19%, according to the Medical Liability Association of New York. But the fixes are clear:- Daily 15-minute team huddles to align on patient priorities.
- Standardized protocols for medication reviews.
- Electronic health records that auto-flag potential generic swaps.
- Collaborative Practice Agreements (CPAs)-legal documents that let pharmacists adjust meds under physician oversight.
The Future Is Integrated
The trend isn’t slowing. The global team-based care market is projected to hit $53.2 billion by 2027. Telepharmacy services have grown 214% since 2020, bringing expert medication review to rural areas where pharmacies are scarce. Even AI is stepping in. Mayo Clinic’s pilot program uses artificial intelligence to suggest generic alternatives based on patient history, insurance coverage, and drug interaction databases. The result? A 22% increase in appropriate generic use and a 9.3% drop in adverse events. And the demand is there. In a 2023 survey, 92% of healthcare executives said they plan to expand team-based medication services. The only question is: will reimbursement catch up? Right now, only 41% of these services are paid at a level that covers their full cost.What Patients Should Expect
If your provider uses team-based care, here’s what you might see:- A pharmacist sitting in the exam room with you-or calling you right after your visit.
- Questions about your medication costs, not just your symptoms.
- Clear explanations about why a generic is safe and effective.
- Follow-up calls or texts to check if you’re taking your meds.
Bottom Line
Generic prescribing isn’t just about saving money. It’s about making sure patients actually get the care they need. Team-based care turns medication management from a fragmented, error-prone process into a coordinated, patient-centered system. It’s not about replacing doctors. It’s about supporting them-with experts who specialize in drugs, adherence, and cost. The evidence is clear: when pharmacists, nurses, and doctors work together, patients take fewer pills they can’t afford, have fewer side effects, and stay healthier longer. And that’s not just good for individuals-it’s good for the whole system.How does team-based care improve generic prescribing?
Team-based care improves generic prescribing by bringing pharmacists-medication experts-into the decision-making process. They review all medications, identify cost-effective generic alternatives, check for interactions, and educate patients. This reduces errors, increases adherence, and lowers out-of-pocket costs. Nurses and care coordinators support by monitoring adherence and ensuring smooth communication between providers.
Who is involved in a team-based care model for medication management?
A typical team includes physicians (for diagnosis and final approvals), pharmacists (for medication reviews and generic substitutions), nurses or medical assistants (for monitoring chronic conditions and patient education), and care coordinators (for communication and record updates). All work under shared protocols and collaborative practice agreements.
Are generic drugs as safe and effective as brand-name drugs?
Yes. Generic drugs must meet the same FDA standards as brand-name drugs. They contain the same active ingredients, dosage, strength, and route of administration. The only differences are in inactive ingredients (like fillers) and packaging. Studies show no meaningful difference in effectiveness or safety for the vast majority of medications.
Can pharmacists prescribe medications in team-based care?
In many states, pharmacists can prescribe or adjust medications under Collaborative Practice Agreements (CPAs) with physicians. These legal agreements define exactly what changes a pharmacist can make-like switching to a generic, adjusting dose, or restarting a stopped med-without needing to consult the doctor each time. This speeds up care and reduces delays.
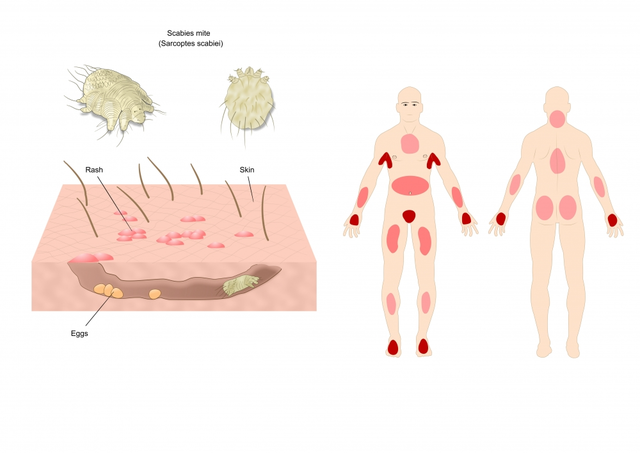
What conditions benefit most from team-based generic prescribing?
Chronic conditions that require long-term, multi-drug regimens benefit the most. This includes hypertension, type 2 diabetes, high cholesterol, asthma, and heart failure. These patients often take five or more medications, making them ideal candidates for comprehensive medication reviews and generic optimization to reduce cost and improve adherence.
Is team-based care covered by insurance?
Medicare Part D plans are required to offer Medication Therapy Management (MTM) services to eligible beneficiaries, and these services are fully covered. Many Medicaid and private insurance plans also cover pharmacist-led medication reviews, especially for patients with multiple chronic conditions. However, reimbursement rates vary, and not all services are fully paid yet.
How long does it take to implement team-based care in a practice?
It typically takes 4-6 months. Month 1-2: Define roles and create protocols. Month 3-4: Update electronic health records to support team communication. Month 5: Train staff (16-24 hours per person). Month 6: Launch a pilot and refine based on feedback. Practices that skip training or fail to integrate technology often struggle with adoption.
What’s the biggest barrier to adopting team-based care?
The biggest barrier is cultural resistance-from providers used to working alone. Other challenges include upfront costs (up to $120,000 per practice for tech and training), inconsistent documentation, and reimbursement gaps. But practices that invest in workflow design and team trust see returns within 12-18 months through reduced hospitalizations and improved patient retention.











11 Comments
Been seeing this in my clinic lately - pharmacists actually sitting in the exam room now. No more waiting a week for a med change. Just one visit, they fix your script, explain why it’s cheaper, and you walk out with a plan. Feels like care finally caught up with reality.
Also, my grandma’s insulin bill dropped from $500 to $90. She’s actually taking it now. That’s not magic. That’s teamwork.
I’m curious - how often do these teams actually *follow up* with patients after switching to generics? I’ve had prescriptions changed before, only to be left hanging with no one checking if the new med actually worked or caused side effects. Is this just another buzzword, or is there real accountability built in?
As a pharmacist who’s been doing this for 12 years - yes, this works. And no, it’s not ‘just a process.’ It’s life-changing. I once had a patient on three brand-name meds for hypertension, diabetes, and cholesterol - $700/month out of pocket. We switched her to generics, coordinated with her nurse to track BP, and had her care coordinator set up a pill organizer. She cried when she saw her first $120 bill. She’s been stable for 18 months now.
It’s not about replacing doctors. It’s about giving them the support they never had. And yes - the data backs it up. Every. Single. Time.
While the concept of team-based care is undeniably sound and grounded in evidence-based practice, one must also consider the systemic implications of shifting responsibility from physicians - who, by virtue of their medical training and licensure, bear ultimate accountability - to pharmacists, nurses, and care coordinators, whose roles, though indispensable, are not legally or ethically equivalent in terms of diagnostic authority. Furthermore, the expansion of Collaborative Practice Agreements across state lines introduces regulatory fragmentation that may compromise patient safety if not uniformly standardized. The economic incentives are compelling, yes - but at what cost to clinical governance? We must not confuse efficiency with efficacy, nor convenience with competence.
And yet - I still believe in the model. Just not without rigorous oversight, standardized protocols, and continuous quality metrics.
My mom’s doctor finally let the pharmacist switch her meds last month. She was on a brand-name statin that cost $400 a month. Now it’s $28. She didn’t even know she could ask. No one ever told her. This isn’t innovation - it’s basic decency. Why does it take a whole team to do what should’ve been standard practice since the 90s?
USA still think they inventing medicine 😂
My cousin in Nigeria - he get generic drugs from India for $5/month. No team. No EHR. No huddle. Just a pharmacy and a man who know what he doing. You guys need 5 people to switch a pill? 🤣
But hey, if it make you feel good about your system - go ahead. We still alive over here with $1 meds.
So now we’re letting pharmacists prescribe? Next thing you know, the pharmacist will be diagnosing your depression, your back pain, and your ‘spiritual imbalance.’
This is socialism creeping into medicine. Doctors used to be the authority. Now we’re turning healthcare into a customer service desk where anyone with a PharmD can ‘adjust’ your meds. What’s next? A TikTok influencer prescribing antibiotics?
And don’t give me that ‘it saves money’ crap. If you’re too poor to afford your meds, maybe you shouldn’t be on them. Stop subsidizing bad life choices with taxpayer dollars.
Love this. Been working with a team like this in Manchester - our pharmacist does med reviews every Tuesday, the nurse texts patients who miss doses, and we’ve got a shared EHR that flags every possible generic swap. We’ve cut our readmissions by nearly a third.
Biggest win? Patients feel seen. Not just ‘another case.’ They’re part of the plan. And honestly? It’s made my job 10x better. No more guessing if they took their pills. We just check the log.
Also - shoutout to the care coordinator who learned to say ‘I got you’ in three languages. That’s the real magic.
Let me get this straight - you’re saying a pharmacist, who went to school for 6 years, knows more about prescribing than a doctor who went to school for 11 years? And you call this progress?
Also, ‘team-based care’ sounds like corporate jargon for ‘we don’t want to pay doctors enough to do their job properly.’
And don’t even get me started on the ‘warm handoff.’ That’s not healthcare - that’s a theme park ride. You get handed off like a hot potato while someone in scrubs tries to upsell you on a cheaper pill.
Wake up. This isn’t innovation. It’s cost-cutting disguised as compassion.
Oh wow. So now the government’s gonna make us all take generics because ‘it’s cheaper.’
Ever heard of bioequivalence? Nah, you didn’t. That’s why Big Pharma invented brand names - so you don’t get sick from some Chinese filler in a pill.
And don’t tell me ‘the FDA says they’re the same.’ That’s the same FDA that let vaping be sold to kids and approved opioids like candy. You trust them with your life? LOL.
My uncle died on a generic. They said ‘same ingredients.’ But his body didn’t like the dye. Turns out, he was allergic to the red #40 in the generic version. No one told him. No one even asked.
Team-based care? More like team-based negligence.
It’s funny, isn’t it? We’ve spent a century building a medical system that treats people like problems to be solved - not humans to be understood.
And now, suddenly, we’re ‘team-based’ because we realized that a person’s health isn’t just a list of vitals - it’s their income, their fear of bills, their ability to read a label, their trust in a system that’s always failed them.
Pharmacists aren’t ‘taking over.’ They’re just doing what doctors never had time to do: listen.
Maybe the real revolution isn’t in the meds we prescribe - it’s in the humility to admit we can’t do it alone.
And if that makes you uncomfortable? Good. You’re supposed to be.