Generic Drug Approval: What Happens Before and After a Generic Hits the Market
When you pick up a generic drug, a lower-cost version of a brand-name medication that contains the same active ingredient, dosage, and intended use. Also known as non-brand medication, it is approved by the FDA only after proving it works just like the original—without needing to repeat expensive clinical trials. But approval isn’t the end. It’s the starting line for ongoing monitoring that affects your safety every time you take it.
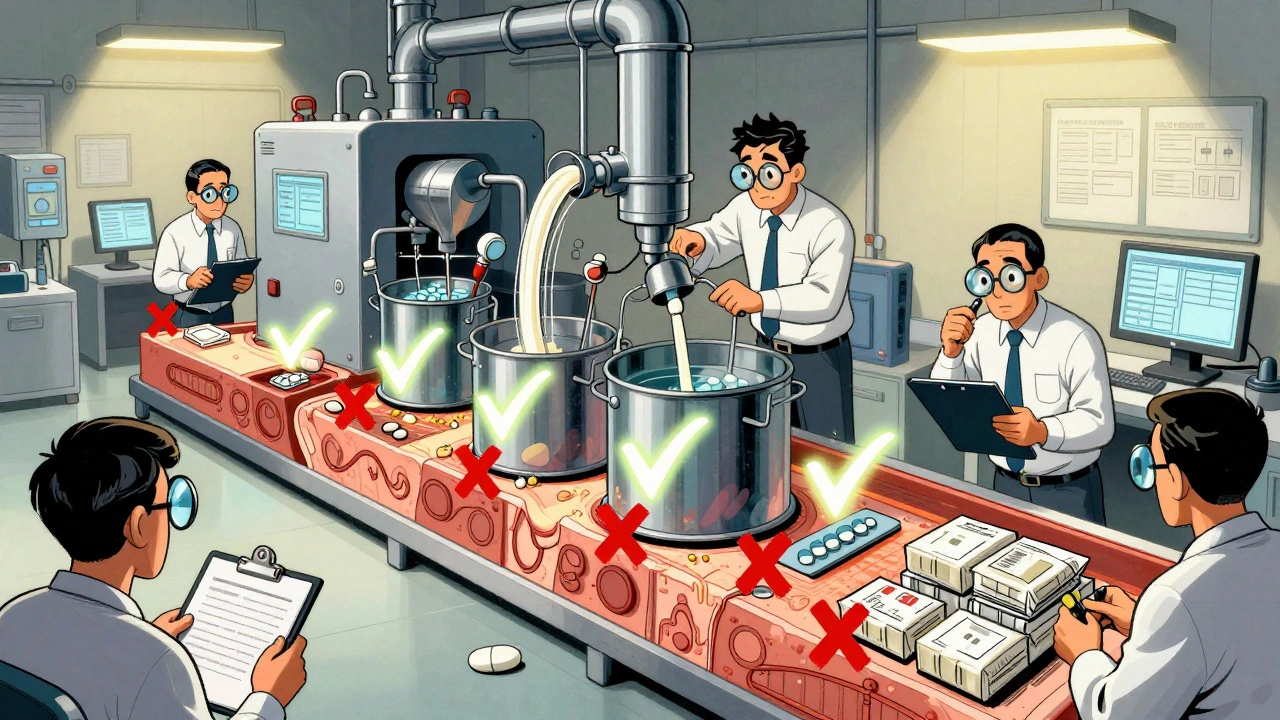
The FDA doesn’t test generics on thousands of people like brand-name drugs. Instead, they rely on bioequivalence, a scientific standard that proves the generic delivers the same amount of active ingredient into your bloodstream at the same rate as the brand. That means your body absorbs it the same way. But here’s the catch: bioequivalence allows for a 20% variation in absorption between batches. That’s legal. That’s normal. But when you’re on a drug with a narrow therapeutic window—like blood thinners or seizure meds—that small difference can matter. That’s why post-market surveillance, the FDA’s system for tracking side effects and problems after a drug is sold to the public. is just as important as the initial approval.
Generics aren’t perfect copies. They can have different inactive ingredients—fillers, dyes, preservatives. These don’t treat your condition, but they can trigger allergies or affect how the drug breaks down in your body. That’s why some people report different side effects with a generic, even when the active ingredient is identical. It’s not in your head. It’s chemistry. And the FDA tracks those reports through systems like FAERS, the same one used for brand-name drugs.
What you won’t hear from pharmacies or ads: multiple generic makers don’t always mean lower prices. Sometimes, when only one company makes a generic, prices stay high. When two or three compete, they drop. But when five or ten make it, some quit because the profit margin is too thin—leaving you with fewer choices and higher costs. That’s why generic drug competition, the number of manufacturers producing the same generic medication. matters more than you think.
And then there’s the human side. Many patients don’t trust generics. They think, "If it’s cheaper, it must be worse." But decades of real-world data show generics work just as well. The problem isn’t science—it’s perception. Doctors and pharmacists can help by explaining what bioequivalence really means, not just saying, "It’s the same."
What you’ll find in these posts is the full picture: how the FDA approves generics, why batch variability happens, what happens when side effects show up years later, how multiple manufacturers affect price, and why some patients have better results with one generic brand over another. You’ll read about real cases where inactive ingredients caused reactions, how Europe keeps generics affordable through transparent bidding, and what you can do if your insurance switches your prescription without telling you. This isn’t theory. It’s what’s happening right now in your medicine cabinet.