COVID-19 Supply Chain: How Drug Shortages, Delays, and Global Risks Affect Your Medications
When the pandemic hit, the COVID-19 supply chain, the global network that moves raw materials, active ingredients, and finished drugs from factories to pharmacies. Also known as pharmaceutical logistics, it isn’t just about shipping boxes—it’s about keeping life-saving medicines flowing when every link is under stress. You might not think about where your pills come from, but when a factory in India shut down or a container got stuck at a port, your blood pressure med or antibiotic could disappear from the shelf. This wasn’t a one-time glitch. It exposed how thin the margins are in drug manufacturing—and how quickly a crisis can turn a small delay into a public health problem.
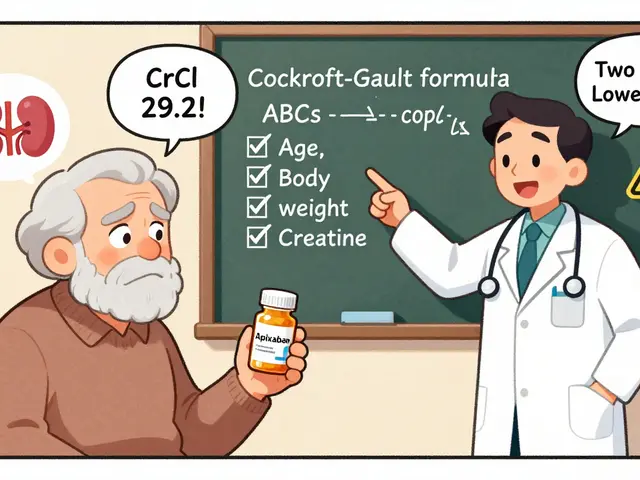
Behind every pill is a chain of suppliers: chemical plants in China make the active ingredients, labs in Europe test them, packaging facilities in the U.S. seal them, and trucks deliver them to your pharmacy. The drug shortages, when medications aren’t available in enough quantity to meet patient needs during the pandemic weren’t random. They came from factory closures, labor shortages, shipping backlogs, and even panic buying. Some generic drugs—like azilsartan or lisinopril—saw spikes in demand as more people needed blood pressure control at home. But if the raw material for those drugs came from a single overseas plant that went offline, production stopped. Even something as simple as the plastic for pill bottles became scarce. And while brand-name drugs had backup suppliers, many generics relied on one source. That’s why generic drug availability, how reliably low-cost versions of medicines reach patients became such a big issue. You were told generics are just as good—but what if you couldn’t get them at all?
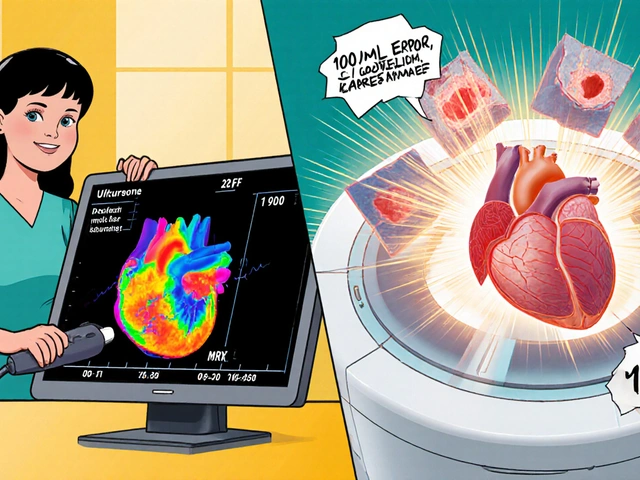
The pharmaceutical logistics, the systems that move medicines across borders with strict temperature, timing, and regulatory controls didn’t just slow down—they broke. Air freight costs jumped. Customs inspections doubled. And when a shipment of molnupiravir or remdesivir got delayed, doctors had to scramble for alternatives. Some patients got switched to different drugs, others waited weeks. Meanwhile, studies showed that even minor delays in antiviral delivery reduced their effectiveness. This wasn’t just about inconvenience—it was about timing. The same supply chain that delivered your monthly prescription also carried the drugs meant to save lives in hospitals. When one part failed, the whole system felt it.
Today, some of those delays are easing, but the risks haven’t disappeared. Factories are still concentrated in a few countries. Labor shortages linger. And if another virus emerges—or a war blocks a key shipping route—you could face the same problem. The COVID-19 supply chain taught us that medicine isn’t just science—it’s logistics. And if you’re taking any long-term medication, you need to know: your pill’s journey is longer and more fragile than you think. Below, you’ll find real stories and data from patients and experts on how these disruptions affected treatments, why some drugs vanished while others didn’t, and what you can do to prepare if it happens again.