COVID-19 Antivirals: What Works, What to Watch For, and How They Affect Your Health
When you hear COVID-19 antivirals, medications designed to stop the SARS-CoV-2 virus from multiplying inside your body. Also known as oral antiviral treatments, they’re meant to be taken early after symptoms start to keep you out of the hospital. These aren’t vaccines—they don’t prevent infection. They’re your backup plan if you get sick and are at risk for severe illness. Drugs like Paxlovid and molnupiravir are the most talked-about options, but they’re not magic pills. They work best when you start them within five days of feeling unwell, and even then, they don’t work for everyone.
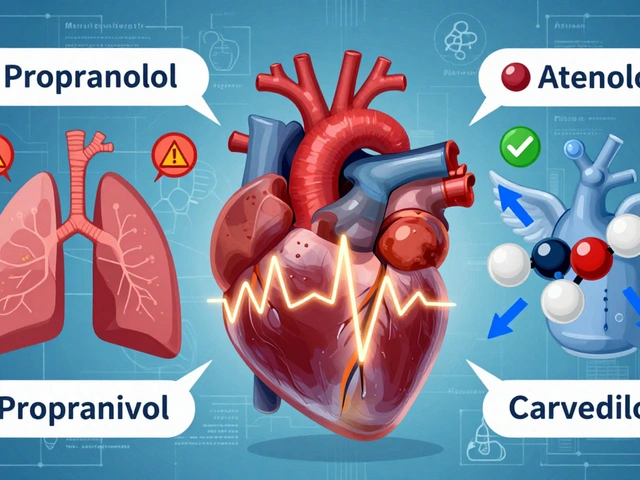
One big reason people can’t get these drugs is drug shortages, when supply can’t keep up with demand during surges. During the worst waves of the pandemic, pharmacies ran out. Even today, if you’re over 65, have diabetes, or heart disease, you might still face delays. That’s not just inconvenient—it’s dangerous. Every hour counts with antivirals. And it’s not just about availability. Some people can’t take them because of drug interactions, how these antivirals react badly with common meds like cholesterol pills or blood thinners. Paxlovid, for example, can’t be mixed with certain statins or antiarrhythmics without serious risk. Pharmacists now check your full list of meds before filling a prescription—not just because of rules, but because lives depend on it.
Then there’s the hidden side effect: stress. If you’re worried about getting the drug in time, or if you’ve been told you’re not eligible, that anxiety alone can make you feel worse. And it’s not just you—health systems were stretched thin. The COVID-19 supply chain, the network of factories, labs, and distributors that make and move these drugs, broke down in places. Pills were made in one country, shipped through another, and held up at borders. That’s why some people got them and others didn’t, even if they were in the same town.
These antivirals aren’t perfect. They’re expensive. They come with nausea, diarrhea, and weird tastes. Some people report brain fog after taking them. But for high-risk patients, the trade-off still makes sense. What you need to know isn’t just whether they work—but whether you can get them, whether they’ll clash with your other meds, and whether you’re in the group that actually benefits. The data is clear: if you’re eligible and act fast, they reduce hospitalization by up to 90%. But if you wait too long, or if your doctor doesn’t know the rules, you might miss your chance.
Below, you’ll find real stories and facts about how these drugs interact with other treatments, why access varies so much, and what you can do to protect yourself if you’re at risk. No fluff. Just what matters when your health is on the line.