Biosimilar Effectiveness: How Well Do They Really Work Compared to Brand Drugs?
When you hear biosimilar, a biologic drug that’s highly similar to an already-approved reference product, with no clinically meaningful differences in safety or effectiveness. Also known as follow-on biologics, these drugs are designed to match the complex structure of original biologic medications like Humira or Enbrel—but at a fraction of the cost. Unlike simple generic pills, biosimilars aren’t exact copies because they’re made from living cells, not chemicals. That’s why their effectiveness isn’t assumed—it’s proven through strict testing. The FDA and EMA require biosimilars to show they work just as well as the original in clinical trials, with matching immune responses, dosing, and patient outcomes.
So why do some people still hesitate? It’s often confusion with regular generics. A biologic drug, a medication made from living organisms, used to treat conditions like rheumatoid arthritis, cancer, and Crohn’s disease is too complex to replicate perfectly, but a biosimilar, a version of a biologic that meets rigorous similarity standards doesn’t need to be identical—it just needs to behave the same in the body. Studies tracking patients on biosimilars for rheumatoid arthritis, psoriasis, and inflammatory bowel disease show no drop in effectiveness over years of use. In fact, real-world data from Europe and Canada, where biosimilars have been used for over a decade, confirms they reduce hospital visits and flare-ups just like the originals.
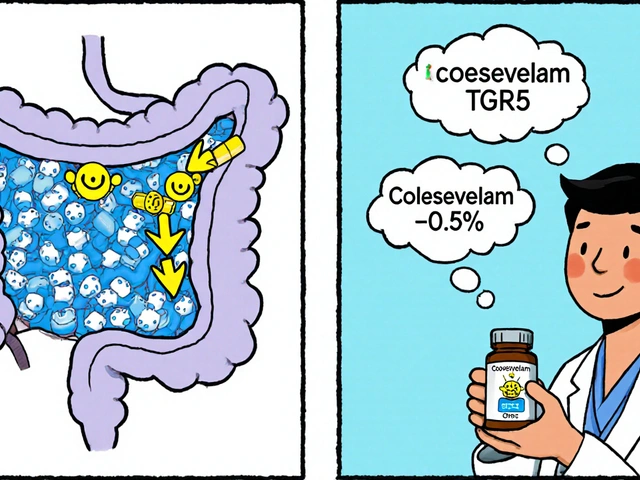
Cost savings are real: biosimilars can cut prices by 30% to 80%, making life-changing treatments accessible to more people. But effectiveness isn’t just about price—it’s about consistency. Batch variability matters, which is why regulators now require tighter controls on manufacturing. Some biosimilars even outperform the original in post-market studies because of improved delivery systems or purification methods. Still, not all biosimilars are created equal. The key is looking at the evidence: look for FDA or EMA approval, check for long-term outcome data, and ask your doctor if the specific biosimilar has been used in your condition.
What you’ll find in the posts below isn’t theory—it’s practical insight from real patients and providers. From how biosimilars stack up against brand-name drugs in autoimmune diseases, to why some doctors still hesitate to switch patients, to what the latest clinical trials say about long-term safety—you’ll see the full picture. No marketing fluff. Just facts you can use to make smarter choices about your treatment.