Generic vs Brand Name Medications: What Really Matters for Your Health
When you pick up a prescription, you might see two names on the bottle: one you recognize, and one that looks like a random string of letters. That’s the difference between a brand-name drug, a medication developed and marketed by a pharmaceutical company under a patent. Also known as originator drug, it’s the version you first hear about from your doctor. And then there’s the generic medication, a copy that contains the same active ingredient, dose, and intended use as the brand version. Also known as nonproprietary drug, it’s often half the price—but does it work the same? The short answer is yes, if it’s approved by the FDA or equivalent agency. But here’s what no one tells you: the real question isn’t whether they work the same—it’s why so many people still doubt them.
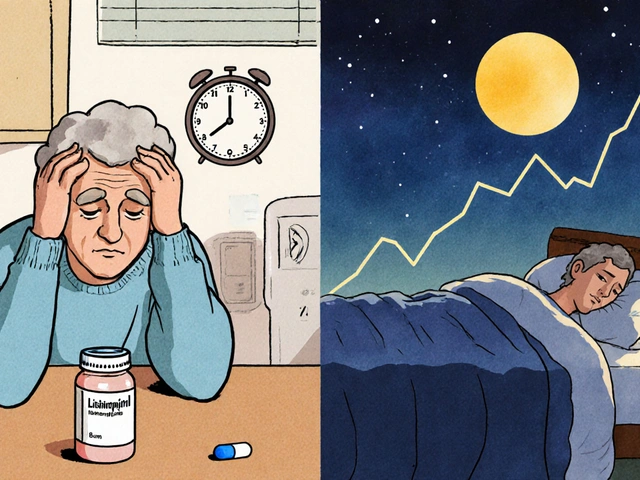
Most people assume brand-name drugs are stronger or safer because they cost more. But the science says otherwise. Both types must meet the same strict standards for bioequivalence, a measure showing the generic version delivers the same amount of active ingredient into the bloodstream at the same rate as the brand. That’s not marketing talk—it’s lab-tested, batch-by-batch proof. Still, some patients feel worse on generics. Why? Sometimes it’s the fillers—the inactive ingredients like dyes or binders—that cause minor reactions. Other times, it’s just the mind playing tricks. A 2020 study in Annals of Internal Medicine found patients reported more side effects on generics… even when they were secretly given the brand-name version. Trust matters as much as chemistry.
And then there’s cost. If you’re paying $150 for a brand-name blood pressure pill and $8 for the generic, it’s not just savings—it’s access. People skip doses because they can’t afford the brand. Generic medications keep millions on treatment. But not all generics are created equal. Some manufacturers cut corners on batch consistency, leading to batch variability, differences in how a drug performs from one production run to the next. That’s why regulators are tightening bioequivalence limits. And why you should always check your pharmacy’s source if you notice a change in how a pill makes you feel.
So what should you do? Talk to your pharmacist. Ask if your generic comes from a reputable manufacturer. Don’t assume all generics are the same. And if you’ve been told generics are "inferior," ask for the data. The truth is, 9 out of 10 prescriptions filled in the U.S. are generics—and most patients do just fine. The real divide isn’t between brand and generic. It’s between those who understand the science and those who’ve been sold a myth.
Below, you’ll find real stories and hard facts from patients and doctors who’ve navigated this choice. From how to safely split pills to why some people feel different switching brands, we’ve gathered the practical insights you won’t find on a drug label. No fluff. Just what works.