Blood Pressure Meds: What Works, What to Watch For, and How to Stay Safe
When you’re on blood pressure meds, prescription drugs used to lower high blood pressure and reduce risk of heart attack or stroke. Also known as antihypertensive drugs, they help your heart and arteries work more efficiently—without you always feeling it. Many people take them daily without thinking twice, but the real story is in the details: which ones work best for you, how they interact with other meds, and what hidden risks might be hiding in plain sight.
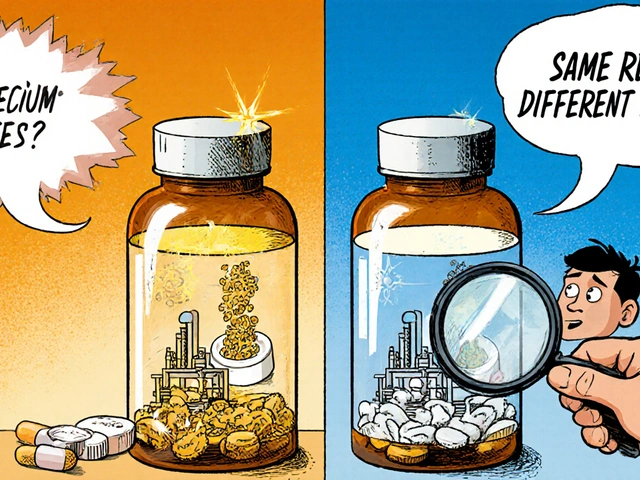
Not all generic blood pressure medication, chemically identical versions of brand-name drugs sold at lower prices. Also known as generic antihypertensives, they’re a smart way to save money—but batch differences and inactive ingredients can still cause unexpected reactions. That’s why some people feel worse on generics, even when their doctor says they’re the same. It’s not always the active drug—it’s the fillers, dyes, or coating that change how your body handles it. And if you’re also taking something like eplerenone, a mineralocorticoid receptor antagonist used for heart failure and high blood pressure. Also known as Aldactone, it’s known to affect bone density over time., you need to know how it might be quietly weakening your bones while protecting your heart.
Then there’s the monitoring side. Taking a pill isn’t enough—you need to know if it’s actually working. That’s where a reliable blood pressure monitor, a home device used to track systolic and diastolic readings over time. Also known as home BP device, it’s one of the most underused tools in managing hypertension. comes in. Without regular checks, you’re flying blind. Maybe your meds are too strong, maybe they’re not strong enough, or maybe your stress, diet, or even electrolyte levels are messing with the numbers. Low potassium? High sodium? Those can undo months of medication. And if you’re splitting pills to save cash, you better know which ones are safe to cut—and which ones could turn dangerous if broken.
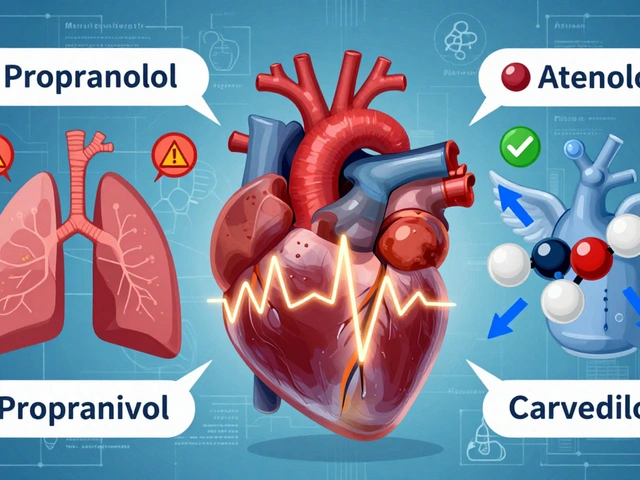
There’s no one-size-fits-all fix. Some people do great on lisinopril. Others need azilsartan. Some need to time their protein intake just right so their meds actually reach the bloodstream. And if you’re on more than one drug, interactions can sneak up on you—especially when you’re mixing generics with supplements or even over-the-counter painkillers. The goal isn’t just to lower the number on the screen. It’s to live without dizziness, fatigue, or weird side effects while keeping your heart safe for the long haul.
Below, you’ll find real, no-fluff guides on exactly what you need to know: how to spot dangerous interactions, why your generic might be acting up, how to use your home monitor properly, and what to do if your meds are affecting your bones, mood, or sleep. No marketing. No fluff. Just what works—and what doesn’t—based on actual patient experiences and medical data.