Biosimilars: What They Are, How They Work, and Why They Matter
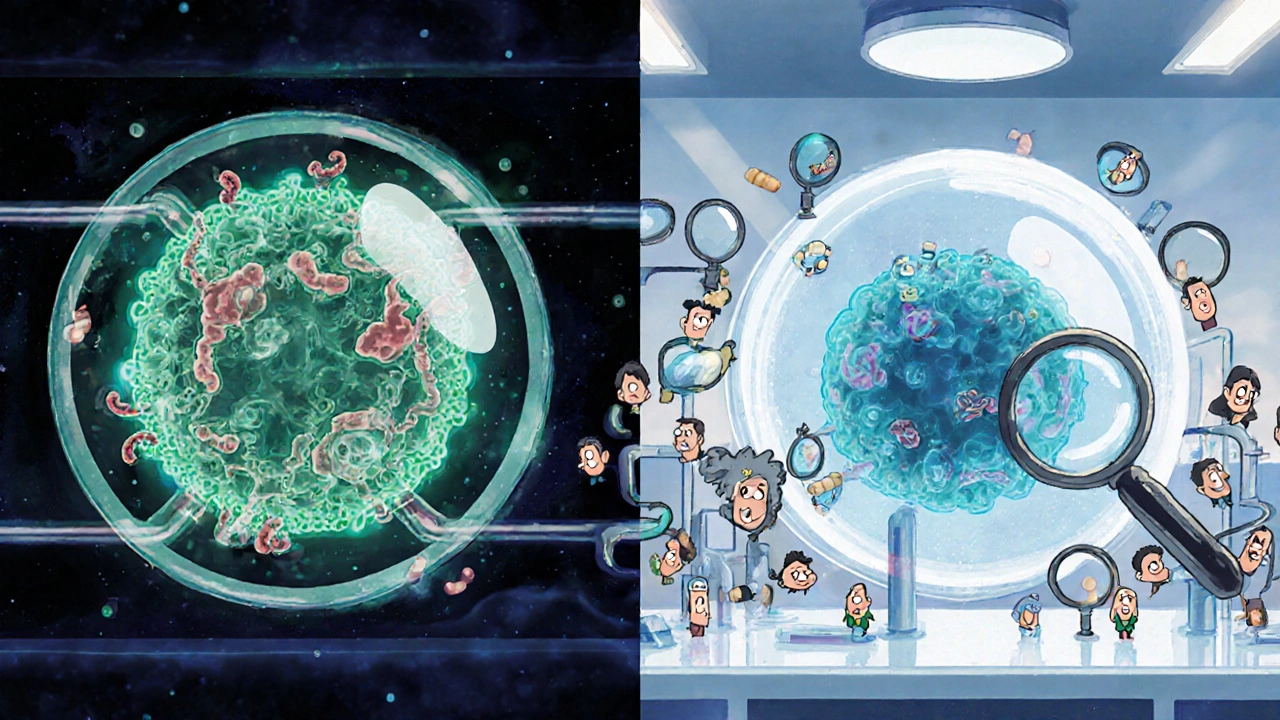
When you hear biosimilars, highly similar versions of complex biologic drugs that are not exact copies but proven to work the same way in the body. Also known as follow-on biologics, they’re the next big thing in affordable medicine. Unlike regular generics that copy simple chemical pills, biosimilars match intricate proteins made from living cells—like antibodies used to treat cancer, arthritis, or diabetes. These aren’t knockoffs. They’re rigorously tested to match the original biologic in safety, strength, and how your body absorbs them.
The real win? Cost. A single course of a brand-name biologic can cost over $20,000 a year. Biosimilars slash that by 15% to 35%, sometimes more. That’s not just savings for insurers—it’s access for patients who couldn’t afford treatment before. But here’s the catch: not all biosimilars are created equal. Some are approved for the exact same uses as the original. Others only cover part of the original’s uses. And while they’re built to be identical in effect, tiny differences in manufacturing can affect how your body responds—especially if you’re switching from the brand name. That’s why post-market studies, like those tracking generic drug safety, how drugs perform after they’re on the market, including rare side effects and long-term outcomes, matter so much. You don’t just take a biosimilar and hope for the best. You track how you feel, report odd symptoms, and work with your doctor to make sure it’s holding up.
It’s not just about price. Biosimilars are reshaping how hospitals buy drugs. In Europe, tendering systems, government-run competitive bidding processes that force drugmakers to lower prices to win contracts have made biosimilars the default choice for public health systems. In the U.S., insurers are pushing them hard—but doctors still face patient skepticism. Why? Because many people think "generic" means "weaker." But science says otherwise. A 2023 FDA review found no meaningful difference in adverse events between biosimilars and their reference products across 12 approved drugs. Still, the fear lingers. That’s why clear communication from pharmacists and doctors is critical. If you’re on a biologic and your pharmacy switches you to a biosimilar, ask: "Is this the same as what I was taking? Will I need more monitoring?" You have the right to know.
What you’ll find below is a collection of real-world guides that cut through the noise. You’ll learn how bioequivalence limits, the acceptable range of variation allowed in how a drug is absorbed and processed by the body are tightening to ensure consistency. You’ll see how post-market surveillance, ongoing monitoring of drugs after approval to catch problems that didn’t show up in clinical trials catches hidden risks in biosimilars. And you’ll get straight talk on how to spot when a switch might affect you—because your health isn’t a cost-cutting experiment. These aren’t theoretical debates. They’re daily decisions made by patients, pharmacists, and doctors who need facts, not marketing.