Biologic Drugs: What They Are, How They Work, and What You Need to Know
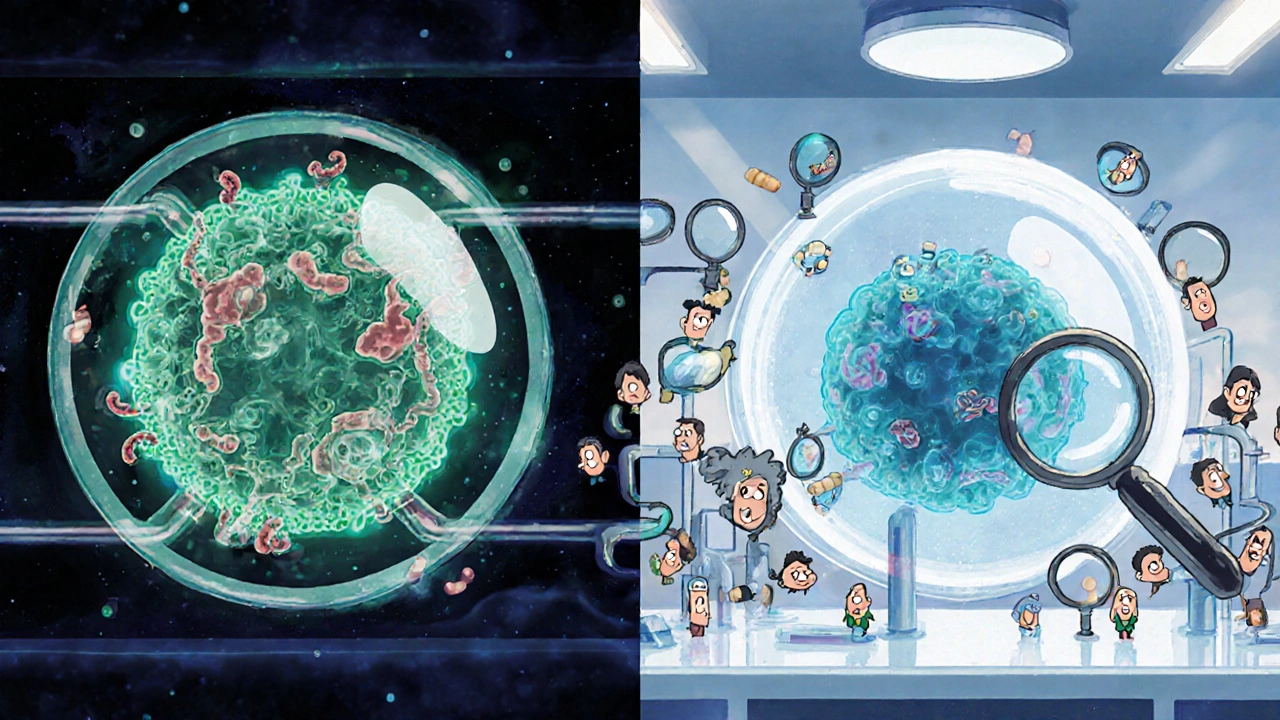
When you hear biologic drugs, complex medicines made from living cells that target specific parts of the immune system. Also known as biologics, they're not like regular pills you swallow—they're injected or infused because your stomach would break them down. These drugs changed how we treat conditions like rheumatoid arthritis, Crohn’s disease, and severe psoriasis by going after the root cause instead of just masking symptoms. Unlike traditional drugs that are chemically synthesized, biologics are grown in labs using living organisms—like yeast, bacteria, or animal cells—which makes them much more complex and harder to copy exactly.
One major type of biologic is monoclonal antibodies, laboratory-made proteins designed to bind to specific targets in the body, like inflammation-causing molecules. These are the backbone of many modern treatments. For example, drugs like adalimumab or infliximab block TNF-alpha, a protein that drives joint damage in arthritis. Then there are biosimilars, highly similar versions of brand-name biologics that come after the original patent expires. They’re not generics—they’re not exact copies—but they offer the same results at lower prices, which is why hospitals and insurers are pushing for them.
Biologics don’t come without risks. Because they quiet down your immune system, you’re more vulnerable to infections like tuberculosis or fungal diseases. That’s why doctors check for latent infections before starting treatment. Some people develop reactions at the injection site, or even rare but serious side effects like nerve damage or heart failure. And while they work wonders for many, they don’t help everyone. If one biologic fails, your doctor might switch you to another with a different target—like one that blocks IL-17 instead of TNF-alpha.
What you won’t find in a pill bottle is how these drugs are handled. They need refrigeration. They often come with special syringes or auto-injectors. Some require weekly shots; others, monthly infusions at a clinic. That’s why patient support programs exist—to help with cost, training, and reminders. And while biologics are expensive upfront, they can cut down on hospital visits, surgeries, and lost workdays, making them cost-effective over time.
Behind the scenes, there’s a lot happening: new biologics are being developed for everything from multiple sclerosis to eczema. The science is advancing fast, and with biosimilars entering the market, access is slowly improving. You’ll see posts here about how to read medication guides for these drugs, what to watch for with side effects, how they interact with other meds, and why timing matters—even if you’re on a biologic for an autoimmune condition, you still need to manage other drugs safely. Whether you’re a patient, caregiver, or just trying to understand why your doctor recommended an injection over a tablet, this collection gives you the real talk—not the marketing.