Antibiotics: What They Are, How They Help, and When to Use Them
If you’ve ever had a bacterial infection, chances are an antibiotic was part of the cure. Antibiotics aren’t magic pills that fight every illness – they only target bacteria, not viruses like colds or flu. Knowing the basics can save you from unnecessary meds and help you get better faster.
How Antibiotics Work
Think of a bacterial cell as a tiny factory. Most antibiotics either smash the factory’s walls or stop it from making essential parts, so the bacteria can’t survive. Penicillin, for example, weakens the wall, while azithromycin blocks protein production. The result is that your immune system clears out the dead bugs with less effort.
When to Take an Antibiotic
You should only start antibiotics when a doctor confirms a bacterial infection. Common situations include strep throat, urinary tract infections, and certain skin wounds. If you have a sore throat that’s actually caused by a virus, an antibiotic won’t help and could cause side effects.
Always finish the full prescription, even if you feel better after a few days. Stopping early lets some bacteria survive, which can lead to resistance – those super‑bugs that are harder to kill later on.
Side effects are usually mild: upset stomach, diarrhea, or a rash. If you notice severe reactions like swelling, trouble breathing, or intense itching, call your doctor right away. Probiotics during or after the course can help keep good gut bacteria balanced.
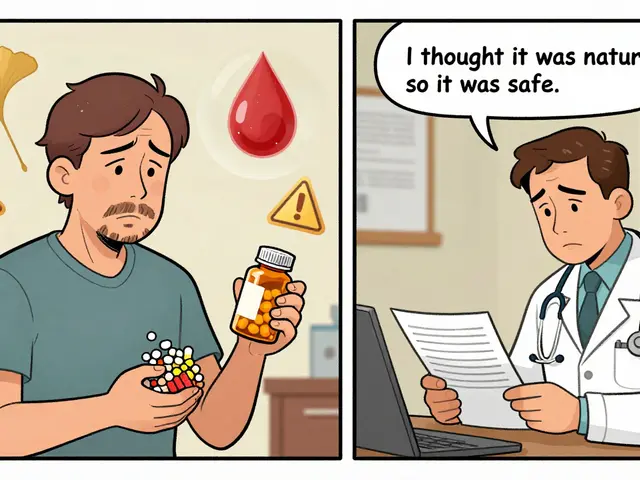
Ask your pharmacist about drug interactions. Some antibiotics don’t mix well with common meds such as antacids, birth control pills, or blood thinners. A quick chat can prevent unwanted surprises.
In short, antibiotics are powerful tools when used correctly. Keep a list of any allergies you have, follow the dosing schedule, and never share your prescription with anyone else. With these simple steps you’ll protect yourself and keep bacteria from getting smarter.