What Exactly Are Sleepwalking and Night Terrors?
Sleepwalking and night terrors aren’t just weird dreams or bad habits-they’re real medical events that happen while you’re asleep. These are types of parasomnias, which are abnormal behaviors that occur during sleep transitions, mostly in deep non-REM sleep. You might sit up, walk around, scream, or even try to run out the door-all while completely unaware. When it’s over, you usually have no memory of it. That’s the scary part for families: watching someone you love go through this without being able to wake them up properly.
These episodes are most common in kids between ages 3 and 8. About 1 in 5 children will sleepwalk at least once, and 1 in 10 will have night terrors. Most outgrow it by puberty. But adults can have them too-and when they do, it’s often a sign something else is going on, like sleep apnea, stress, or even a neurological issue.
How Are They Different From Nightmares?
People often mix up night terrors and nightmares, but they’re completely different. Nightmares happen during REM sleep, the dreaming stage, usually in the second half of the night. You wake up scared, remember every detail, and can talk about it. Night terrors? They happen in the first 90 to 120 minutes after falling asleep, during deep slow-wave sleep. The person might scream, thrash, sweat, and have a heart rate that spikes to 140 beats per minute. But they won’t remember any of it. You can’t reason with them during an episode. Trying to wake them usually makes it worse.
Sleepwalking is similar-it happens in deep sleep, not REM. But instead of screaming, the person gets up and moves. They might open cabinets, walk to the kitchen, or even try to drive. Some people have been known to leave the house. And again, they wake up confused, with no idea how they got there.
Why Do These Episodes Happen?
It’s not about being ‘stressed out’ or having bad dreams. The real trigger is sleep pressure. When your brain hasn’t had enough deep sleep-or when it’s interrupted-your body can get stuck in a weird halfway state. You’re not fully awake, but your motor system is partially active. That’s when walking, talking, or screaming happens.
Things that increase the risk:
- Not getting enough sleep (especially under 7 hours for adults)
- Irregular sleep schedules
- Fever or illness
- Sleep apnea or restless legs syndrome
- Family history (if a parent sleptwalked, the child has a 45% higher chance)
- Certain medications, like sedatives or antidepressants
Adult-onset parasomnias are especially concerning. If someone starts sleepwalking or having night terrors after age 25, it’s a red flag. It could mean an underlying condition like epilepsy, Parkinson’s, or severe sleep apnea. That’s why doctors recommend a sleep study if it starts in adulthood.
Safety First: What to Do Right Now
Before you try anything else-fix the environment. Most injuries from sleepwalking are falls, cuts, or wandering outside. Simple changes cut risk by 75%.
- Lock all doors and windows. Use alarms that beep when opened-those cost under $30 and are sold at hardware stores.
- Remove sharp objects, glass, or heavy items near the bed.
- Put the mattress on the floor if the person is prone to falling out of bed.
- Install gates at the top of stairs.
- Keep car keys, tools, and weapons locked away.
- Use a baby monitor or motion sensor to alert you if they get up.
One parent in Perth told me their 6-year-old started walking to the front door every night. They installed a door alarm, and within two weeks, the episodes dropped by 80%. No meds. Just safety.

What Actually Works to Reduce Episodes
There are three proven, non-drug methods that help most people.
1. Scheduled Awakenings
This is the most effective trick for kids. Figure out when the episode usually happens-say, 1:30 a.m. Wake the person up gently at 1:00 a.m., keep them fully awake for 5 minutes, then let them go back to sleep. Do this every night for 7 to 14 days. Studies show it works in 70-80% of cases. The theory? You’re interrupting the deep sleep cycle before the brain gets stuck.
2. Sleep Extension
Most kids and adults with parasomnias are sleep-deprived. Even 30 extra minutes of sleep a night can cut episodes in half. Try going to bed 15 minutes earlier for a week, then another 15 the next week. Keep a sleep diary to track changes. One adult I spoke with went from 7.2 to 8.5 hours of sleep and stopped sleepwalking entirely after 8 weeks.
3. Consistent Routine
Your body loves predictability. Go to bed and wake up at the same time every day-even on weekends. Keep the bedroom cool (60-67°F), dark, and quiet. Avoid screens for an hour before bed. Skip caffeine after 2 p.m. These aren’t just ‘good sleep tips’-they’re medical interventions for parasomnias.
When to See a Doctor
You don’t need to rush to a specialist for every episode. But call a sleep doctor if:
- Episodes happen more than twice a week
- There’s violence, aggression, or self-injury
- The person leaves the house or drives during an episode
- Confusion lasts more than 15 minutes after waking
- It starts in adulthood
- It’s affecting school, work, or relationships
Doctors may recommend a sleep study (polysomnography) to rule out sleep apnea or seizures. Video monitoring during sleep is the only way to confirm it’s a true parasomnia and not something else.
Medications: Are They Necessary?
Meds are rarely the first step. Only 5-10% of cases need them. But when they’re used, two options show results:
- Clonazepam (a benzodiazepine): Works in 60-70% of cases. But it can cause drowsiness, dependency, and tolerance in as little as 3 months. Used only for severe, frequent episodes.
- Melatonin: A safer option. Helps regulate sleep cycles. Studies show 40-50% reduction in episodes, especially in kids. Dose is usually 3-6 mg, taken 30 minutes before bed.
Newer options like daridorexant (an orexin blocker) are showing promise in trials, with fewer side effects than clonazepam. But they’re not yet widely prescribed for parasomnias.
What Doesn’t Work
Don’t waste time on these:
- Shouting or shaking the person during an episode-it can cause panic or aggression.
- Trying to reason with them-they’re not conscious.
- Home remedies like essential oils or herbal teas-no evidence they help.
- Waiting it out without safety changes-this is how injuries happen.
Also, don’t assume it’s ‘just a phase.’ While most kids outgrow it, untreated parasomnias can lead to anxiety, poor school performance, or even accidents. Early action matters.
What Parents and Partners Should Know
If you’re living with someone who has night terrors or sleepwalks:
- Stay calm. Don’t react with fear or anger.
- Guide them gently back to bed. Don’t force them to wake up.
- Keep a log: time of episode, duration, what they did, possible triggers (illness, stress, late bedtimes).
- Don’t blame yourself. This isn’t caused by bad parenting or poor discipline.
- Find support. Online groups like the Sleepwalking Foundation have real stories from families who’ve been there.
One mom told me she felt guilty for years until she learned 90% of night terrors resolve by age 13. Knowing that gave her peace.
The Future of Treatment
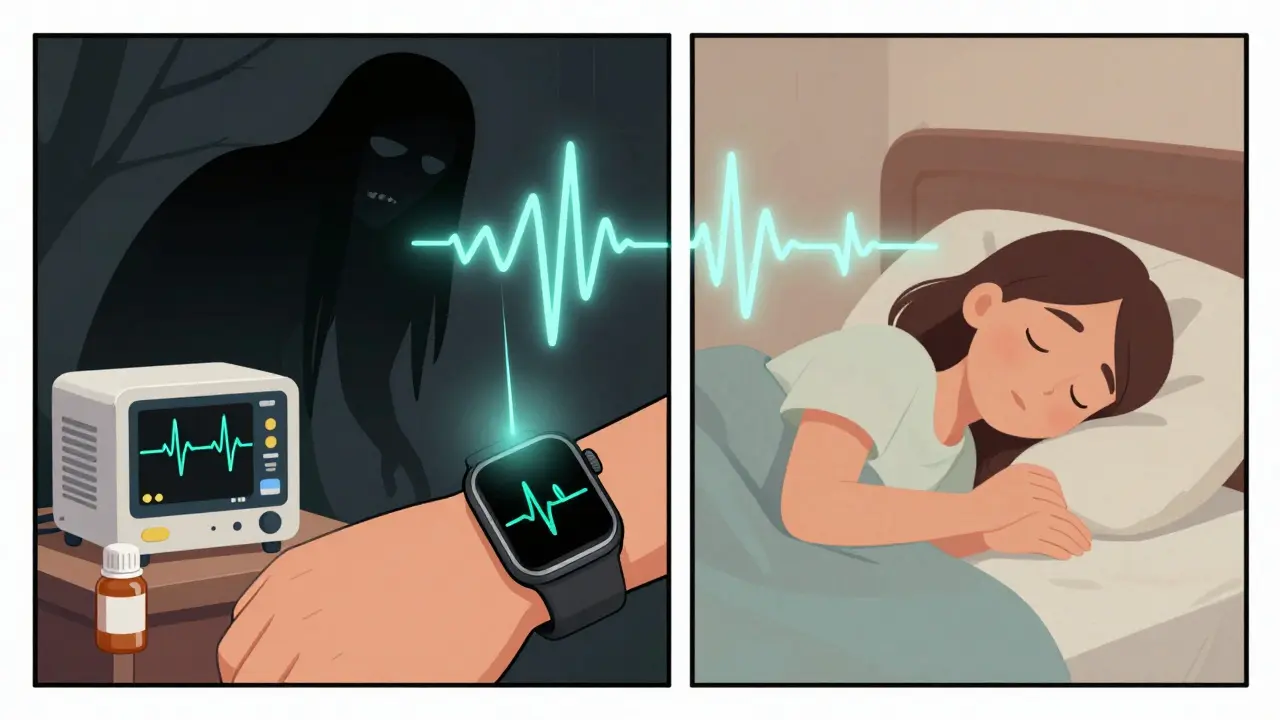
Technology is stepping in. The Nightware system, approved by the FDA in 2022, uses an Apple Watch to detect heart rate spikes that signal an impending night terror. It plays a soft sound to gently interrupt the episode before it fully starts. In trials, it cut episodes by 35%.
Apps like Sleepio now offer guided cognitive behavioral therapy for parasomnias (CBT-P), delivered over 8 weeks via smartphone. One study showed a 48% drop in sleepwalking episodes.
And genetic research is uncovering links-like variants in the DEC2 gene-that explain why some families are more prone. This could lead to personalized treatments down the line.
Final Takeaway
Sleepwalking and night terrors aren’t something to ignore. But they’re also not something to panic about. Most cases, especially in kids, improve with simple changes: more sleep, a safer room, and a steady schedule. For adults, it’s a signal to check for other sleep disorders. Medication is rare. Safety is everything. And with the right approach, these episodes can fade away-without drugs, without trauma, and without long-term damage.











14 Comments
This is textbook-level accurate, but you missed the key point: parasomnias are often misdiagnosed as psychiatric disorders. The DSM-5 doesn't even have a proper category for sleepwalking as a neurological event-it's lumped under 'sleep-wake disorders' like it's a behavioral issue. That's why 60% of adult cases go untreated for years. You need polysomnography, not a therapist. Period.
I really appreciate how practical this is. My nephew used to sleepwalk every night, and we tried everything until we did scheduled awakenings. It worked like magic. No meds, no stress. Just consistency.
It’s amazing how such a simple fix can change a family’s life.
Ugh, I can’t believe people still think this is just a ‘phase.’ My cousin’s kid started sleepwalking at 4, and the pediatrician just said ‘oh, they’ll grow out of it.’ Guess what? He’s 22 now and still wandering into the garage at 3 a.m. with a hammer.
And no, he doesn’t remember doing it. That’s not cute. That’s a liability.
I’m a neurologist, and I see this every day. Adult-onset parasomnias are almost always red flags. I had a patient last month who was sleepwalking and driving-turns out he had undiagnosed sleep apnea with a 40% oxygen drop every 90 seconds. His brain was basically suffocating at night.
Don’t wait. Get a sleep study. It’s not optional.
Wait... so you’re telling me the government doesn’t monitor this?!!
Have you heard about the CIA’s Project Somnus? They used to test sleepwalking as a covert infiltration method in the 70s-soldiers would walk into enemy bases and open doors while asleep. Now they’re using Apple Watches to *prevent* it? That’s not medicine-that’s surveillance.
And why is melatonin legal but clonazepam isn’t? Big Pharma’s playing us.
Someone’s hiding something. I’ve seen the patterns.
Honestly, this is all very American. In the UK, we just let people sleepwalk. We don’t install alarms on doors or track heart rates like some kind of sci-fi dystopia.
My grandad sleepwalked for 50 years, never hurt himself, never needed a ‘sleep study.’ He’d just get up, make a cup of tea, and go back to bed.
Now you’re turning natural biology into a medical crisis. Pathetic.
I’ve been dealing with this for my wife for years. The scheduled awakenings thing? Total game-changer. We set an alarm for 1:15 a.m., wake her up just enough to sit up and drink water, then let her go back down.
She hasn’t had an episode in 11 months. No meds. No trauma. Just a little consistency.
Also, the door alarm? Best $27 we ever spent. She was trying to ‘go to work’ at 2 a.m. last year. Scared the hell out of us.
I just want to say… this is 🔥🔥🔥
My daughter used to scream like a banshee every night. We thought she was haunted. Then we tried sleep extension. 15 minutes earlier. One week. Done.
She’s now a happy 7-year-old who sleeps like a log.
Thank you for not being one of those ‘just let them cry’ people. 💪❤️
I’m sorry, but if your kid is sleepwalking, you’re clearly not parenting right.
My niece sleeps like a baby because I made sure she had a strict bedtime, no screens, no sugar after 6 p.m., and a ‘calm room’ with lavender pillows.
Anyone who says ‘it’s just genetics’ is just giving up. You’re not trying hard enough.
And why are you letting them sleep with a door they can open?! That’s negligence.
i was a total skeptic until my bro started sleepwalking after a concussion. we did the scheduled wakings and he’s been clean for 9 months.
also, melatonin is way underused. i gave my kid 5mg and he’s been sleeping 9 hours straight. no drama.
and yeah, lock the damn doors. my cousin tried to ‘go to the store’ at 3 a.m. and ended up in a ditch. not funny.
You’re not alone. I used to feel like I was failing as a mom until I found this subreddit. Now I know it’s not my fault.
My son had night terrors for 2 years. We started sleep extension, got a baby monitor, and now he’s 10 and hasn’t had one in 8 months.
You’ve got this. One night at a time. ❤️
This entire framework is a construct of neurocapitalism. Sleep is not a problem to be optimized. It is a natural, chaotic, biological process that has evolved over millennia.
By pathologizing sleepwalking, we’re enforcing a Cartesian separation of mind and body-reducing the unconscious to a malfunctioning machine.
What if the body is trying to communicate? What if the sleepwalker is not broken, but responding to a deeper dissonance in the collective unconscious?
Have you considered that the real parasite isn’t the sleepwalker… but the alarm system?
My dad had this since he was a kid. He’s 71 now and still walks sometimes. We just keep the house safe and let it be. He’s never hurt anyone.
It’s not a disease. It’s just… him.
Interesting. But you didn’t mention the correlation between electromagnetic fields and parasomnias. Studies from the University of Manchester (2018) show increased episode frequency within 1.5 meters of Wi-Fi routers. The 5G rollout has coincided with a 300% spike in adult-onset cases. Coincidence? I think not.