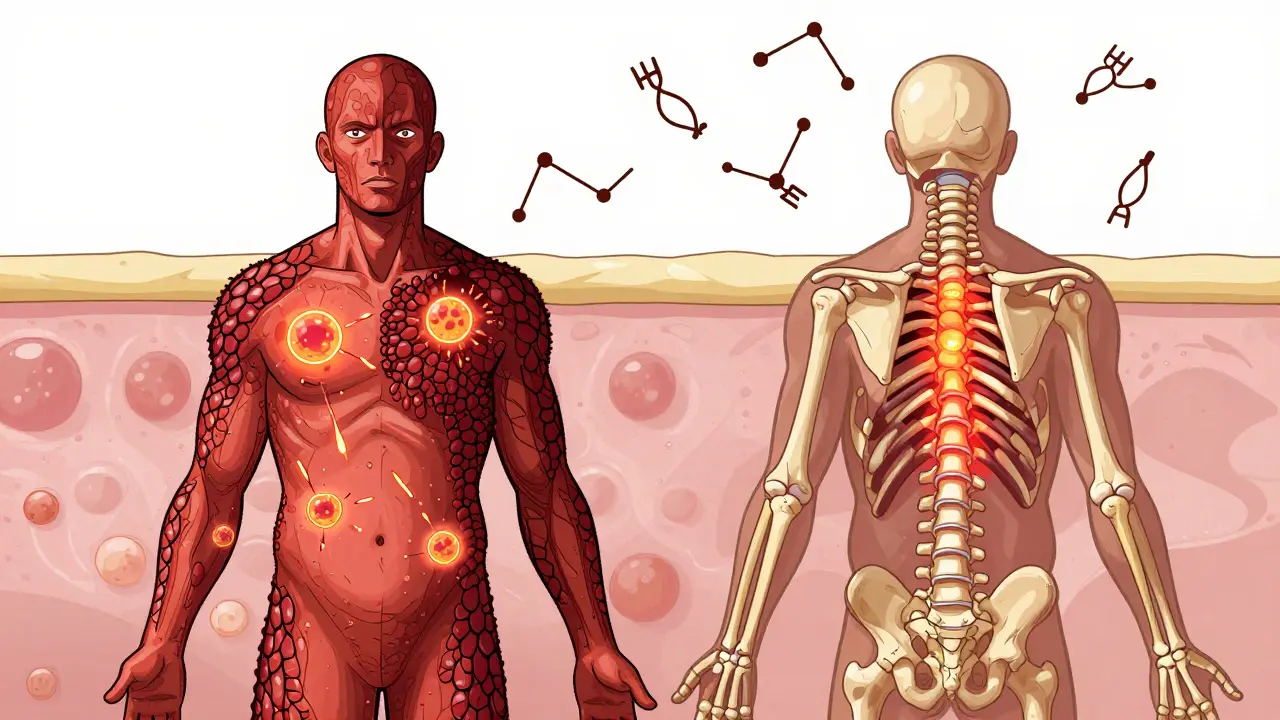
When your skin breaks out in red, scaly patches, it’s easy to think it’s just a cosmetic issue. But if those patches come with stiff, swollen fingers, aching heels, or lower back pain, you’re not dealing with just a skin condition-you’re facing psoriatic arthritis, a full-body autoimmune attack. About 1 in 3 people with psoriasis will develop it. And for many, the joint damage starts quietly, long before they realize something’s wrong.
How Psoriasis Turns Into Psoriatic Arthritis
Psoriasis isn’t just dry skin. It’s your immune system mistakenly targeting healthy skin cells, causing them to multiply too fast. That’s what creates those thick, silvery plaques. But in up to 30% of cases, the same immune chaos doesn’t stop at the skin. It spreads to joints, tendons, and even the spine. That’s psoriatic arthritis (PsA).The shift from skin-only to joint involvement isn’t random. Genetics play a big role. People with HLA-B27, HLA-B38, or HLA-B39 genes are far more likely to develop PsA. But genes alone don’t cause it. Stress, infections, obesity, or even injury can trigger the immune system to turn on joints. For most, psoriasis shows up first-often years before the joints hurt. But in 5 to 10% of cases, the joints swell before the skin ever breaks out. That’s why doctors now look for psoriasis in the nails, even when the skin looks fine.
The Hidden Signs: More Than Just Swollen Fingers
Many people think arthritis means stiff knees or aching hips. PsA is different. It doesn’t always follow the classic pattern. Here’s what it really looks like:- Dactylitis: One or more fingers or toes swell up like sausages. It’s not just a sore joint-it’s the whole digit inflamed. About 4 in 10 PsA patients have this.
- Enthesitis: Pain where tendons meet bone. Think Achilles tendon pain or the bottom of your foot hurting when you step out of bed. This happens in 35 to 50% of cases.
- Nail changes: Pitting, thickening, or nails lifting off the nail bed. Eight out of 10 PsA patients have this. It’s often the earliest clue.
- Back pain: Not from lifting something heavy. This is inflammatory back pain-worse in the morning, improves with movement, and doesn’t go away with rest. It’s often linked to the spine.
- Joint damage: X-rays show bone erosion in 60 to 70% of long-term cases. Some even develop ‘pencil-in-cup’ deformities, where bone wears away on one side and grows abnormally on the other.
These aren’t random symptoms. They’re signs your immune system is attacking multiple parts of your body at once. That’s why diagnosing PsA requires looking at the whole picture-not just the skin or the joints, but both.
How Doctors Diagnose It: The CASPAR Criteria
There’s no single blood test for PsA. Instead, doctors use a system called CASPAR, developed in 2006 and still the gold standard today. To confirm PsA, you need inflammatory joint disease plus at least three of these:- Current psoriasis (3 points)
- History of psoriasis (2 points)
- Nail pitting or separation (1 point)
- Negative rheumatoid factor (1 point)
- Characteristic bone changes on X-ray (1 point)
A score of 3 or more means PsA. The system is 99% accurate at ruling out other types of arthritis like rheumatoid arthritis. That’s critical-because treatment is totally different.
Doctors also use blood tests to check for inflammation markers like CRP and ESR, but these can be normal even when damage is happening. Imaging is key. Ultrasound can spot early swelling in tendons. MRI shows bone inflammation before X-rays do. And yes, sometimes a skin biopsy is done-not to diagnose psoriasis, but to rule out eczema or fungal infections that look similar.

Treatment: Stopping the Attack Before It’s Too Late
The goal isn’t just to reduce pain. It’s to stop joint damage before it’s permanent. That’s why treatment starts early and targets the immune system directly.For mild cases, NSAIDs like ibuprofen help with pain and swelling. But they don’t stop the disease. If symptoms stick around, doctors move to methotrexate-a traditional DMARD that slows immune activity. It works for about half of patients, but not everyone.
For moderate to severe PsA, biologics are the game-changer. These are injectable or infused drugs that block specific parts of the immune system:
- TNF inhibitors (adalimumab, etanercept): First-line for spine and tendon pain. About 50-60% of patients see at least a 20% improvement.
- IL-17 inhibitors (secukinumab, ixekizumab): Better for skin and nails. Often preferred if psoriasis is worse than joint pain.
- IL-23 inhibitors (guselkumab, risankizumab): Newer, with long-lasting results. Already showing promise in early trials.
- JAK inhibitors (tofacitinib, deucravacitinib): Oral pills that block internal immune signals. Great for people who hate needles.
There’s no one-size-fits-all. The choice depends on what’s hurting most-your skin, your back, your fingers. If you have mostly skin issues, IL-17 blockers win. If your spine is stiff, TNF inhibitors are stronger. And if you’ve tried one and it stopped working, there’s usually another that will.
What Success Looks Like: Minimal Disease Activity
The new standard isn’t just ‘feeling better.’ It’s achieving minimal disease activity (MDA). That means:- 1 or fewer tender joints
- 1 or fewer swollen joints
- Psoriasis covering 1% or less of your skin
- Pain score under 15/100
- Quality of life score under 20/100
- HAQ disability score under 0.5 (meaning you can still do daily tasks without help)
- No fatigue
It’s ambitious. But studies show that if you hit MDA within 6 to 12 months, you’re far less likely to need joint replacements or suffer permanent damage. The goal isn’t just to manage symptoms-it’s to get your life back.
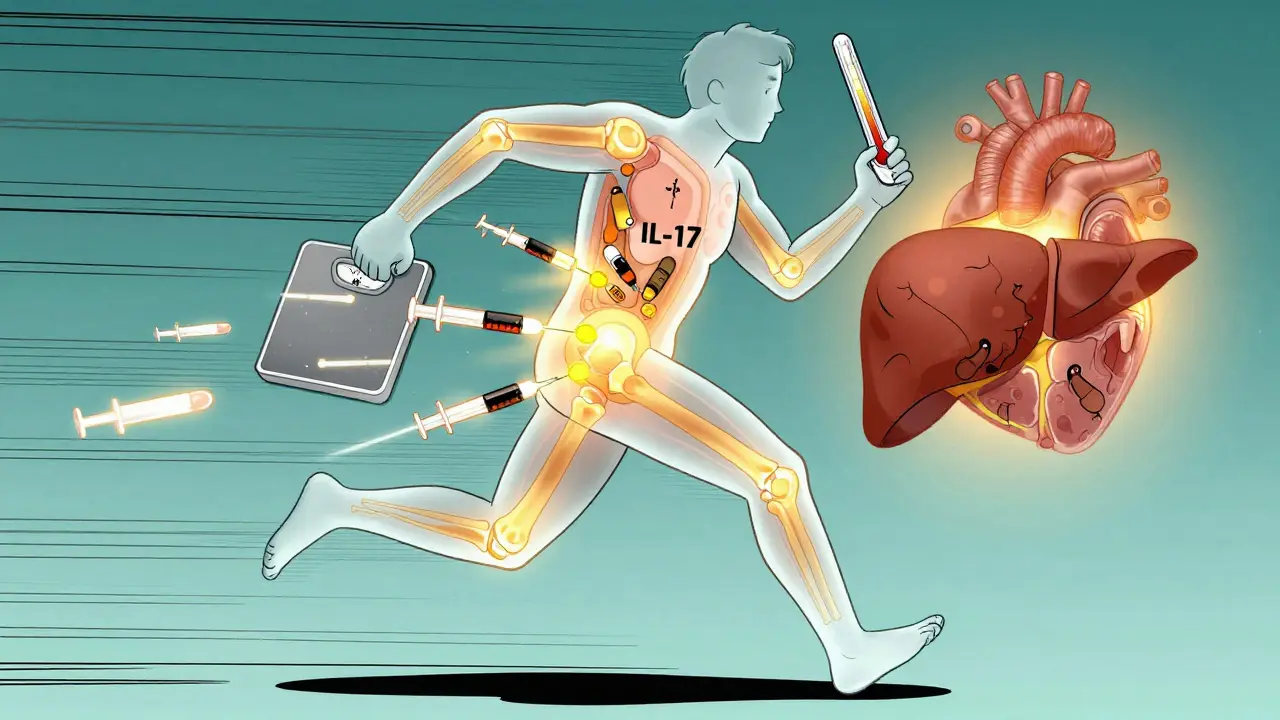
The Silent Risks: Comorbidities No One Talks About
PsA isn’t just a skin and joint disease. It’s a systemic condition that raises your risk for other serious problems:- Heart disease: 40-50% of PsA patients have metabolic syndrome. Your risk of heart attack is 43% higher than someone without it.
- Depression and anxiety: 1 in 3 people with PsA report symptoms. The constant pain, appearance changes, and fatigue wear you down.
- Diabetes and fatty liver: Linked to chronic inflammation and obesity, both common in PsA.
- Early death: Studies show PsA patients die 30-50% sooner than average-mostly from heart problems.
That’s why treatment now includes checking your blood pressure, cholesterol, and blood sugar. Your rheumatologist should ask about your mood. If you’re struggling with depression, therapy or medication isn’t optional-it’s part of your care plan.
What’s Next: The Future of PsA Care
Research is moving fast. Scientists are finding that gut bacteria differ in PsA patients-suggesting diet or probiotics might help down the line. New blood tests for calprotectin and MMP-3 could soon tell us who’s likely to progress, so we can treat before damage starts.By 2027, experts predict 70% of PsA patients will be on biologics or targeted pills within two years of diagnosis. That’s up from 40% today. The message is clear: early, aggressive treatment saves joints, saves lives, and saves quality of life.
If you have psoriasis and notice new joint pain-even if it’s just your fingers feeling stiff in the morning-don’t wait. See a rheumatologist. Don’t assume it’s just aging. Don’t think it’s ‘not that bad.’ The sooner you act, the more of your life you keep.
Can psoriasis cause joint damage even if I don’t have pain?
Yes. Up to 40% of people with psoriatic arthritis have joint inflammation without noticeable pain. That’s why imaging like ultrasound or MRI is important-even if you feel fine, hidden damage can be happening. Regular check-ups with a rheumatologist can catch this early.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. While both are autoimmune and cause joint swelling, rheumatoid arthritis usually affects small joints symmetrically (both hands, both knees) and tests positive for rheumatoid factor. Psoriatic arthritis often affects joints unevenly, causes dactylitis and enthesitis, and is linked to psoriasis and nail changes. The treatments overlap but aren’t identical.
Can I stop taking my medication if my skin clears up?
No. Clear skin doesn’t mean the immune system has calmed down. Stopping treatment can trigger flare-ups and lead to irreversible joint damage. Even if you feel fine, continuing medication is essential to prevent long-term harm. Always talk to your doctor before making changes.
Does weight loss help with psoriatic arthritis?
Yes. Losing even 5-10% of body weight can reduce joint pain, improve medication effectiveness, and lower inflammation markers. Obesity makes PsA harder to control and increases heart disease risk. Weight management isn’t optional-it’s part of treatment.
Are biologics safe for long-term use?
They’re generally safe when monitored. The biggest risk is increased infection, so doctors screen for TB and hepatitis before starting. Regular blood tests check liver and immune function. Most people tolerate them well for years. The risk of not treating-permanent joint damage, heart disease, disability-is far greater than the risks of the medication.











8 Comments
Thank you for this comprehensive breakdown. As someone who’s been managing psoriatic arthritis for over a decade, I can confirm that early intervention made all the difference. I ignored my stiff fingers for months thinking it was ‘just aging’-until I couldn’t button my shirt. The moment I saw a rheumatologist, my life changed. Biologics weren’t a cure, but they gave me back my mobility. Don’t wait for pain to be ‘bad enough.’ Your future self will thank you.
Also, nail changes? I had them for years before the joints flared. No one ever mentioned it. This post should be mandatory reading for anyone with psoriasis.
And yes-weight loss helped more than any drug. Losing 12% of my body weight cut my CRP in half. It’s not a magic fix, but it’s non-negotiable.
Keep pushing for early diagnosis. We’re not just patients-we’re advocates now.
Let’s be real-this article reads like a pharmaceutical ad with footnotes. Biologics cost $20,000 a year. Most people can’t afford them. The ‘minimal disease activity’ goal sounds great until you’re on Medicaid and your rheumatologist only sees you once a year.
And don’t get me started on ‘gut bacteria’ being the next miracle cure. We’ve had 12 years of ‘the microbiome will save us’ and zero practical applications. This is feel-good medicine wrapped in jargon. Real talk: if you can’t afford treatment, you’re screwed. No amount of ‘early intervention’ changes that.
Also, ‘pencil-in-cup’ deformities? That’s not a clinical term-it’s a radiology joke. Stop romanticizing destruction.
Just wanted to say this is one of the clearest, most compassionate explanations of PsA I’ve ever read. I was diagnosed last year after years of misdiagnosis-first as ‘overuse injury,’ then ‘fibromyalgia.’ The nail pitting was the clue no one noticed. I thought it was just bad manicures.
What really hit home was the part about depression being part of treatment. I didn’t realize how much the fatigue and isolation were affecting me until I started therapy. It’s not weakness-it’s part of the disease.
And yes, weight loss helped. Not because I ‘should’ve lost weight sooner,’ but because my body finally stopped fighting itself. I’m not ‘cured,’ but I’m living again. Thank you for normalizing this journey.
Ugh. Another one of these ‘psoriasis is an autoimmune monster’ scare pieces. Look, if you’re overweight, sedentary, and eating sugar like it’s going out of style, no biologic is going to save you. The real problem isn’t the immune system-it’s your lifestyle.
I’ve seen 30 patients this month with PsA. 28 of them had BMI over 35. Guess what? They all got worse after starting biologics because they kept eating donuts.
Stop blaming your genes. Stop chasing expensive drugs. Eat real food. Move your body. Sleep. That’s the ‘treatment.’ Everything else is just window dressing.
And if you’re too lazy to do that, don’t act like you’re a victim. You chose this.
There’s a fundamental flaw in the CASPAR criteria: it assumes psoriasis precedes arthritis. But what about the 5–10% where joints inflame first? The system is designed to confirm, not discover. That’s why patients with isolated enthesitis or dactylitis are misdiagnosed as having reactive arthritis or fibromyalgia for years.
Furthermore, the reliance on HLA-B27 is outdated. Recent studies show only 45% of PsA patients carry it. The rest are being excluded from early diagnosis because we’re clinging to a 1980s genetic model.
And let’s not pretend JAK inhibitors are ‘safe.’ The FDA black box warning for cardiovascular death isn’t a footnote-it’s a headline. We’re trading one risk for another without long-term data.
This isn’t medicine. It’s algorithmic triage disguised as science.
Interesting. But where’s the data on long-term remission? You mention MDA as a goal, but what percentage of patients sustain it beyond five years? And what happens when biologics lose efficacy? Most papers only track outcomes for 12–24 months.
Also, the claim that ‘70% of patients will be on biologics by 2027’ assumes universal access. In the UK NHS, wait times for rheumatology referrals are 18 months. How does that align with ‘early aggressive treatment’?
This reads like a US-centric marketing pamphlet. Outside of private healthcare, most of this is theoretical.
Man. I read this and felt seen. I had psoriasis since I was 16. At 28, my left heel started screaming every morning. I thought it was my shoes. Turned out it was enthesitis. No pain, just… stiffness. Like my body was full of rust.
Got the diagnosis after my nail started lifting-looked like someone peeled off a sticker. My dermatologist didn’t even blink. Said, ‘Oh, that’s psoriasis.’ I said, ‘But my foot hurts.’ He shrugged. Two years later, I’m on secukinumab and my toes don’t look like sausages anymore.
And yeah, the depression? Real. I stopped hanging out with friends because I didn’t want to explain why I couldn’t lift a grocery bag. Therapy didn’t fix my joints, but it fixed my soul.
Don’t wait for the pain to scream. Sometimes it just whispers. Listen.
Also-weight loss? I dropped 30 lbs. Not because I was told to. Because I wanted to feel like me again. Not a walking autoimmune textbook.
Thank you for writing this. As someone who’s been on a TNF inhibitor for four years, I can say with certainty that the fear of side effects is often worse than the reality. I was terrified of infections-I canceled vacations, avoided crowds, panicked over every sniffle.
Turns out, the biggest risk was doing nothing.
My joints are stable. My skin is clear. I’m back to hiking and playing with my kids. The medication isn’t perfect, but it’s the bridge between surviving and living.
And yes-my rheumatologist checks my blood pressure, cholesterol, and mood every visit. It’s not just about the joints. It’s about the whole person.
If you’re reading this and hesitating? Please, don’t wait. You’re not being dramatic. You’re not overreacting. You’re just finally listening to your body.