Market Competition in Pharmaceuticals: How Generic Drugs, Pricing, and Trust Shape Your Choices
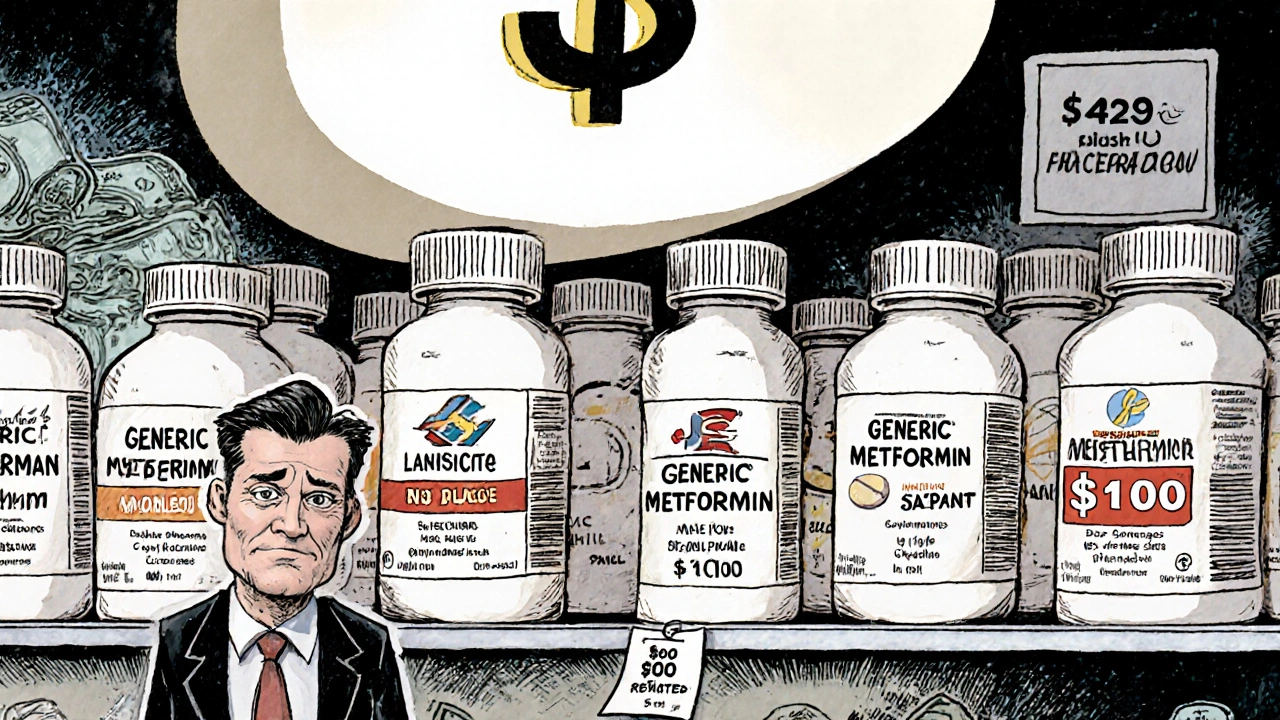
When you buy a medication, you’re not just choosing a drug—you’re stepping into a complex system shaped by market competition, the clash between drug makers over price, access, and patient trust. Also known as pharmaceutical pricing pressure, it’s what pushes generic drugs into pharmacies and keeps brand-name drugs expensive. This isn’t just corporate strategy—it’s personal. Your ability to afford, trust, and stick with your meds depends on who’s winning this fight.
Behind every generic pill is a battle over bioequivalence, the science proving a generic works just like the brand. Also known as generic drug equivalence, this concept is the foundation of market competition in prescriptions. But bioequivalence alone doesn’t win trust. Patients still worry that generics are weaker, less reliable, or even unsafe—often because of batch variability, when different production runs of the same generic behave slightly differently. Also known as pharmacokinetic variability, it’s a real issue that companies are now tightening standards to fix. Meanwhile, drug shortages, supply chain cracks, and patent games keep prices high and choices limited. The pharmaceutical supply chain, the network that moves drugs from factories to your medicine cabinet. Also known as medication availability system, it’s been tested by pandemics, geopolitical shifts, and profit-driven hoarding. When a drug vanishes, people suffer. When a generic floods the market, prices drop—but so does confidence if quality feels inconsistent.
It’s not just about money. Market competition also forces doctors and pharmacists to explain why a $5 generic is just as good as a $150 brand. That’s why posts here cover team-based care, patient trust, and how to split pills safely to cut costs. You’ll find real stories about how people navigate these pressures—like switching blood pressure meds to nighttime dosing to avoid dizziness, or using herbal alternatives to avoid expensive prescriptions. You’ll see how religious fasting affects dosing, how opioid laws change driving behavior, and why a black box warning on antidepressants might have done more harm than good. This isn’t theory. It’s what happens when profit, policy, and patient needs collide.
What you’ll find below isn’t just a list of articles—it’s a map of how market competition actually plays out in real lives. From the chemistry of inactive ingredients to the psychology of trust, these posts show you how to spot the real risks, cut through the noise, and make smarter choices with your health.