Generic Drug Interactions: What You Need to Know Before Taking Them
When you take a generic drug, a medication that contains the same active ingredient as a brand-name drug but is sold under its chemical name. Also known as generic medications, it works the same way in your body—but that doesn’t mean it’s always safe to mix with other pills you’re taking. Many people assume because a generic drug is cheaper and approved by the FDA, it can’t cause unexpected reactions. That’s a dangerous myth. Generic drug interactions happen just like they do with brand-name drugs, and sometimes they’re harder to spot because you’re not paying attention to the name on the bottle.
One big reason this gets overlooked is bioequivalence, the standard that proves a generic drug performs the same as the brand version in your bloodstream. But bioequivalence doesn’t mean every batch behaves exactly the same under every condition. Small differences in fillers, coatings, or release rates can change how a drug interacts with food, alcohol, or other medications. For example, if you’re on a blood pressure pill like lisinopril and start taking a new generic version, the timing of when you take it could suddenly make you dizzy—especially if you’re also on a diuretic or a cholesterol drug. That’s not the brand-name drug failing. It’s the interaction between the generic version and your other meds.
And it’s not just about what’s in the pill. Your body’s chemistry matters too. If you have kidney problems, liver disease, or are over 65, your system processes drugs slower. A generic version that works fine for your neighbor might overload your system. That’s why medication safety, the practice of understanding how all your drugs work together to avoid harm isn’t just for brand-name users. It’s critical for anyone on generics. Studies show that nearly 40% of older adults take five or more medications, and most of those are generics. The risk of dangerous overlaps—like mixing a generic statin with a generic muscle relaxant—is real.
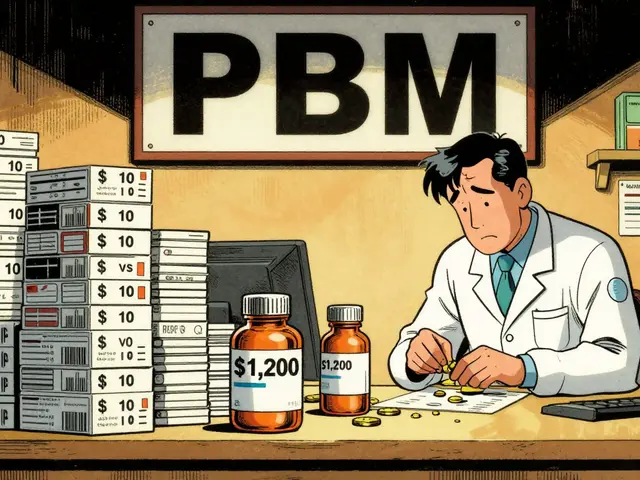
You might think your pharmacist has it all figured out, but even they can miss interactions if you don’t tell them about every supplement, OTC painkiller, or herbal product you’re using. Things like St. John’s Wort, calcium supplements, or even grapefruit juice can turn a harmless generic into a problem. And if you’re splitting pills to save money—something we’ve seen in posts about pill splitting—that changes how the drug is absorbed. A half-tablet might not release the same way as a whole one, especially with extended-release generics.
What you’ll find below isn’t a list of scary warnings. It’s a practical collection of real stories and science-backed advice from people who’ve been there. From how eplerenone affects bone density while interacting with other heart meds, to why high-protein meals block levodopa absorption in Parkinson’s patients taking generics, these posts cut through the noise. You’ll learn when timing matters, which combinations to avoid, and how to talk to your doctor without sounding paranoid. No fluff. No fearmongering. Just clear, usable info to help you take control of your meds—no matter the price tag.