Biosimilar Safety: What You Need to Know About Generic Biologics
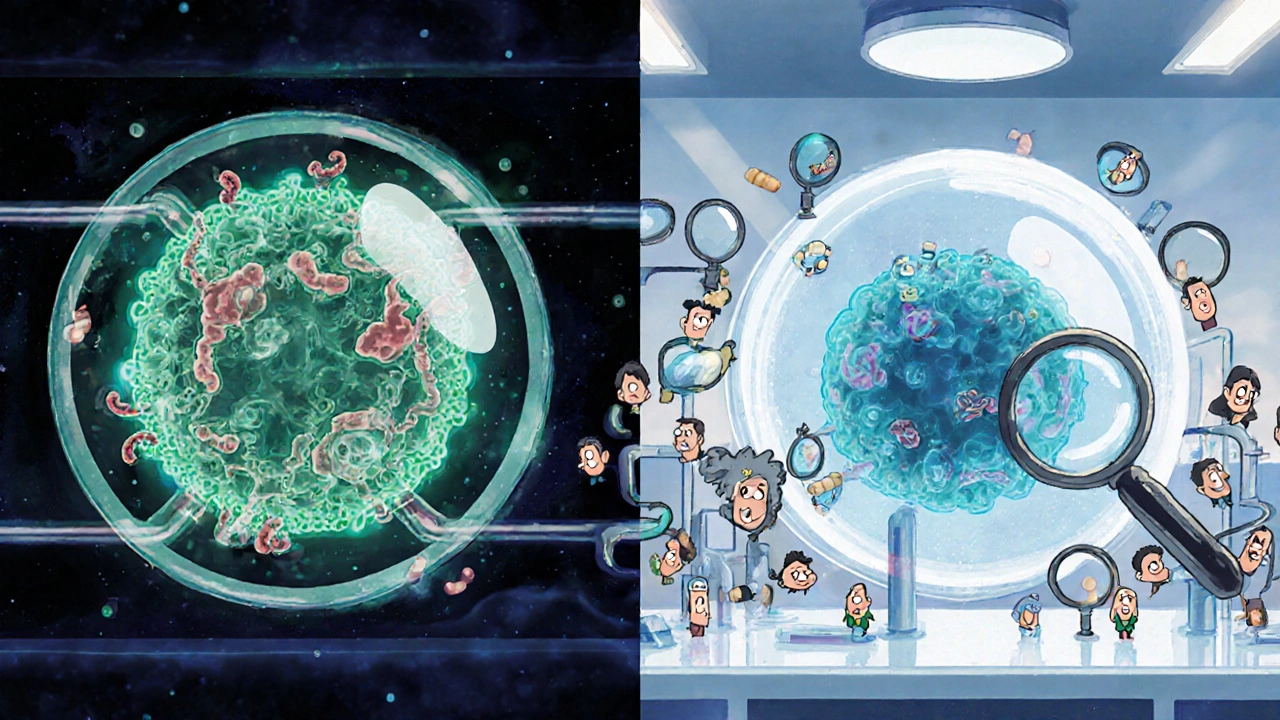
When you hear biosimilar, a biological medication that is highly similar to an already-approved brand-name biologic, with no clinically meaningful differences in safety or effectiveness. Also known as generic biologics, they are not exact copies like small-molecule generics—they’re made from living cells, which makes their production far more complex. But that doesn’t mean they’re riskier. The FDA and EMA require strict testing to prove they work the same way, cause the same side effects, and have the same safety profile as the original. What most people don’t realize is that biosimilars, biological drugs developed to match reference products after patents expire have been used safely in Europe for over 15 years and in the U.S. for more than a decade. Millions of patients with rheumatoid arthritis, Crohn’s disease, and cancer have switched without increased harm.
Still, questions linger. Why do some patients worry about switching? It’s often because of confusion with regular generics. Unlike pills, biological medications, complex proteins derived from living organisms, such as insulin, monoclonal antibodies, or growth factors can’t be perfectly replicated. Tiny differences in manufacturing—like cell line, storage, or purification—can affect how the body responds. That’s why regulators don’t just compare lab results. They look at real-world outcomes: hospital visits, immune reactions, and long-term side effects. Studies tracking patients on biosimilars for up to seven years show no new safety signals compared to the original drugs.
One major concern is immunogenicity—whether the body develops antibodies against the drug. This can reduce effectiveness or cause allergic reactions. But the same risk exists with the original biologic. The key difference? Biosimilars are tested for this specifically before approval. If a biosimilar triggers more immune responses than the reference product, it doesn’t get approved. Post-market surveillance catches rare issues, just like with any drug. The FDA and EMA require companies to monitor adverse events, and many countries have systems that track which exact product a patient received, down to the batch number.
What you won’t find in most headlines is how drug safety, the ongoing evaluation of a medication’s risks and benefits in real-world use works after approval. It’s not a one-time check. It’s continuous. If a biosimilar causes unexpected side effects, regulators can pull it, issue warnings, or require additional studies. And because biosimilars are often cheaper, more patients get access—meaning more data gets collected faster. That’s not a weakness. It’s a strength.
You’ll see posts here that dig into how post-market studies track hidden risks in generics, how drug interactions can surprise you even with approved meds, and how patient trust in cheaper drugs is built through transparency—not marketing. You’ll find real examples of what happens when dosing changes, when switching drugs, or when side effects show up months later. This isn’t theory. It’s what patients and doctors are dealing with right now.