Drug Pricing: Why Medications Cost What They Do and How to Save
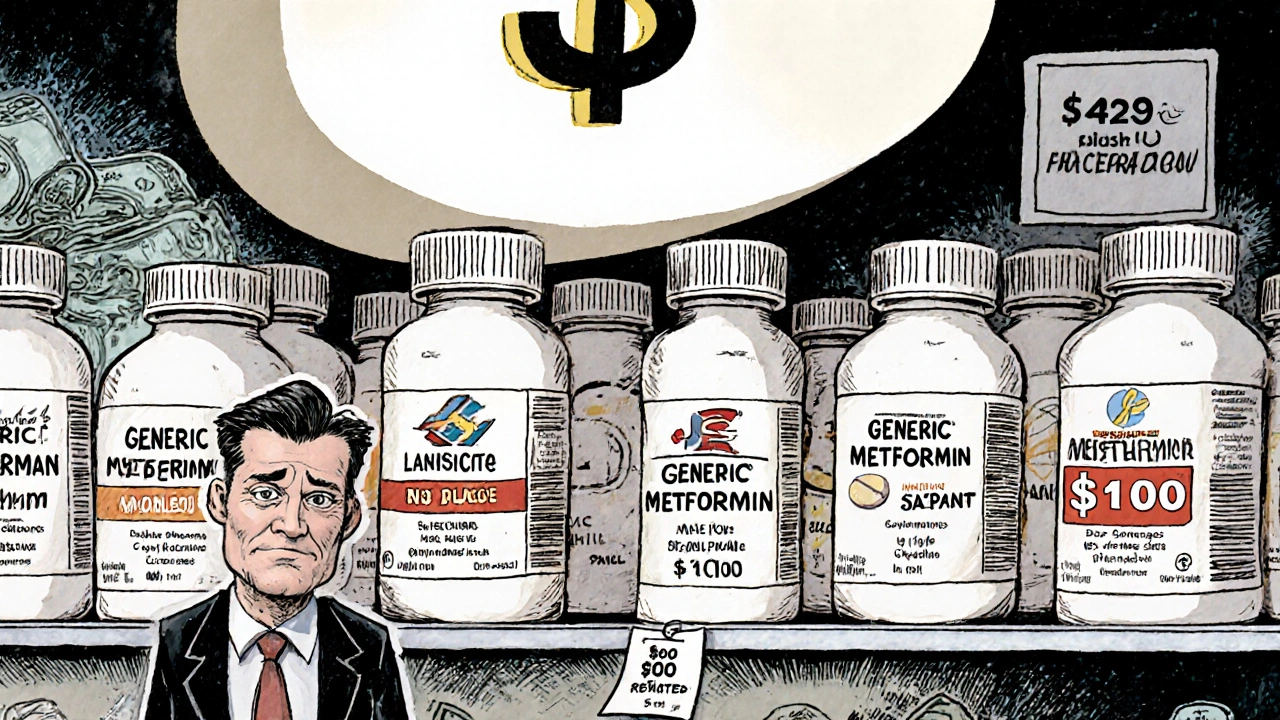
When you pick up a prescription, the price can feel random—sometimes it’s under $10, other times it’s over $500. That’s drug pricing, the system that determines how much you pay for a pill, injection, or cream, shaped by patents, manufacturing, insurance, and market control. It’s not just about the active ingredient—it’s about who owns the rights, how long they’ve had them, and whether a cheaper version is allowed on the market yet. Many people assume brand-name drugs are better, but generic drugs, medications with the same active ingredient as brand-name versions, approved by the FDA as equally safe and effective. Also known as generic equivalents, they often cost 80% less. Yet, even generics can be expensive if you’re paying cash, or if your insurance doesn’t cover them well. That’s where understanding medication costs, the total out-of-pocket expense including copays, deductibles, and what you pay without insurance becomes critical.
Drug pricing isn’t just about the pill in your hand—it’s tied to how it’s made, who sells it, and even when you take it. For example, prescription affordability, how easy or hard it is for patients to access needed meds without financial strain is affected by batch variability, pharmacy benefit managers, and even whether your doctor knows about pill-splitting options. You can save hundreds a year by splitting certain tablets safely, switching to a generic, or timing your dose to avoid costly brand-name upgrades. Some meds, like blood pressure pills, work just as well—or better—when taken at night, and that timing can mean the difference between paying for a brand or sticking with a $5 generic. Meanwhile, drug shortages, like those during the pandemic, pushed prices up overnight when supply couldn’t keep up with demand. And while you might hear about drug companies raising prices for "research," the real issue is often lack of competition. Once a patent expires, dozens of manufacturers can make the same drug, and prices usually drop fast—but not always, because of how insurance and pharmacy networks are set up.
What you’ll find below are real, practical ways people are cutting their drug bills without risking their health. From how to split pills safely to understanding why a generic might still cause side effects due to inactive ingredients, these posts cut through the noise. You’ll see how team-based care—doctors, pharmacists, nurses working together—helps steer patients toward cheaper, equally effective options. You’ll learn how to spot when a drug’s cost is inflated by marketing, not medicine. And you’ll get clear comparisons: is Rumalaya worth it over turmeric? Is Liv.52 better than milk thistle? These aren’t theoretical questions—they’re daily decisions that add up to hundreds or thousands saved per year. This isn’t about avoiding meds. It’s about getting the right ones at the right price.