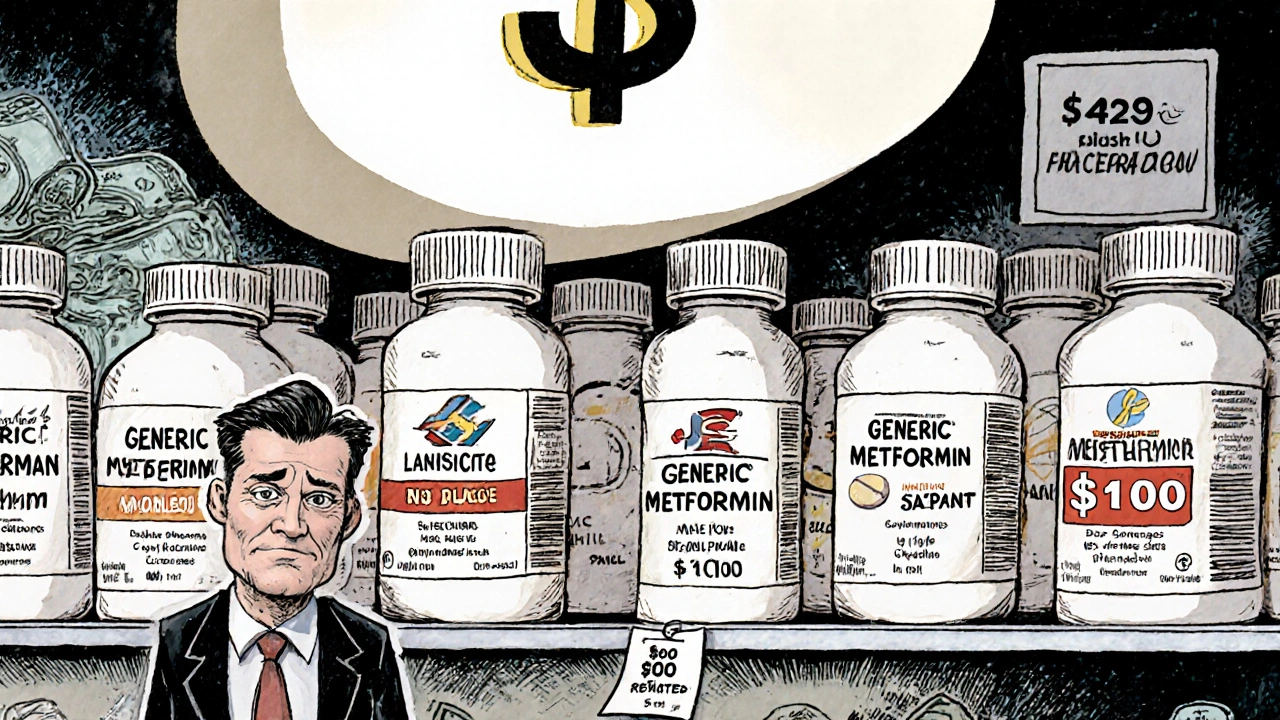
Generic Drug Competition: How Market Forces Shape Prices, Trust, and Access
When you pick up a generic drug, a medication that contains the same active ingredient as a brand-name drug but is sold under its chemical name. Also known as off-patent medication, it is the backbone of affordable healthcare in the U.S. and beyond. The moment a brand-name drug loses its patent, multiple manufacturers jump in—each making the same pill at a fraction of the cost. This is generic drug competition, the market-driven process where multiple producers offer identical or near-identical medications, forcing prices down. It’s not just about savings—it’s about access. Millions rely on generics to manage high blood pressure, diabetes, depression, and more. Without this competition, many couldn’t afford their meds at all.
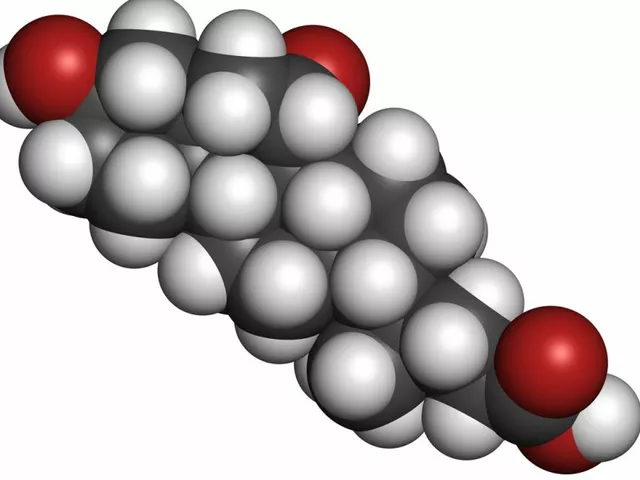
But competition isn’t always clean. While the active ingredient must match the brand, the inactive ingredients, the fillers, dyes, and binders that hold the pill together. Also known as excipients, they can vary between manufacturers and sometimes trigger unexpected reactions. That’s why some patients feel a difference—even though science says they shouldn’t. Bioequivalence, the standard that ensures a generic drug performs the same way in the body as the brand. is measured by how fast and how much of the drug enters the bloodstream. The FDA allows small variations—up to 20%—in absorption. For most people, that’s fine. But for drugs with narrow therapeutic windows—like blood thinners or seizure meds—those tiny differences matter. That’s where batch variability, the natural differences between production runs of the same generic drug. becomes a real concern. One batch might work perfectly; the next might cause dizziness or a flare-up. It’s not a flaw in the system—it’s a limitation of chemistry.
And then there’s trust. Many patients still believe generics are "weaker" or "inferior," even though studies show they work just as well. That doubt doesn’t come from science—it comes from marketing, misinformation, or a bad experience with a specific batch. Doctors and pharmacists play a big role in fixing this. When a pharmacist explains why the pill looks different but does the same job, or when a doctor says, "I prescribe generics to my own family," it changes minds. Generic drug competition isn’t just about price wars—it’s about building confidence. The posts below dig into exactly that: how team-based care improves prescribing, why some patients hesitate to switch, how pill splitting saves money without risk, and what the latest data says about consistency across batches. You’ll find real stories, practical tips, and clear science—no fluff, no hype, just what you need to make smart choices about your meds.